– Good morning, thank you all for coming today to listen to the presentation on Agriculture and Whole Health Wellness for Veterans. I’d like to talk about the VI pilot program that the William S. Middleton Memorial Hospital has started. This pilot program will help veterans with their healthcare, their reintegration into community and into work, and also assist the agricultural vocations in our community at large. My name is Denise Chapin. I am the transitional vocational services program manager with Madison VA Hospital, and I have been in the field of vocational rehabilitation for about 13 years now. For those of you who are not familiar with what vocational rehabilitation is, it’s a program that assists people with disabilities or barriers to employment to get back into work. And that is something that the VA holds dearly to them.
So today I am going to talk about the intersection between agriculture, healthcare, and human services. And then, how we developed the VA Pilot Program to match healthcare trends and vocational needs of veterans and the vocational needs of farmers in our community. And then I’d like to end my presentation with the VA,
the VA using the Whole Health model of care, and how that is empowering veterans to take control of their healthcare needs.
So, how did we get to this unique intersection between agriculture, healthcare, and human services? So, as I mentioned, the VA hospital has a program called compensated work therapy. It’s a program that works with veterans who have challenges, either physical, mental, or emotional, and we help them obtain meaningful competitive employment in the community while also receiving necessary and appropriate services from the VA. But we didn’t always focus on agriculture as a therapeutic strategy at the VA. This is something very new to us. And that is what I wanted to start out and explain, where this model of care came from.
So the history of care farming came about in the 1970’s in Europe, and really gained popularity in Europe as being an innovative and effective way to address healthcare needs of veterans and people with disabilities. So care farming is also called green farming and social farming, and it’s the use of people with disabilities, in the past it was mostly people with developmental disabilities, maybe mental illness, substance use dependence or even youth who are involved in the juvenile justice system, and they had a chance to get their therapy on a farming setting. Could be horticulture, it could be working with animals, a variety of different settings. And, it was found that participants in this care farming strategy had a significant decrease in depression, anxiety, and perceived stress levels. And at the same time, they had an increase in coping skills, self-esteem, attention span, and their ability to be self affecting.
So, in addition to that, participants in care farming found that they had an increased level of connectedness with others, especially in horticultural environments where they may be working side by side with other people, where in the past they may have isolated and not wanted to get out and socialize. They found that agricultural therapy helped them do that.
And they also had a sense of meaningfulness for the community. So the work they were doing was giving back to their community and they had a sense of caring for mother nature.
So the history of care farming in Europe is currently supported by their healthcare system. They have– Their insurance covers it. It’s like getting a prescription to get therapy in an agricultural setting. It’s considered, again, an innovative healthcare strategy for individuals who have various barriers and disabilities. But it didn’t always come at a time when healthcare was funding and supporting care farming. It came at a time when funding for healthcare was low in Europe and there weren’t a lot of options for people that needed care. Likewise, it came at a time in Europe where farming, farms and agriculture, were struggling and they were having a hard time getting by. It makes me think about today, in our agriculture in the United States, it’s struggling and that we have a lot of unique ways that farmers are diversifying and innovating their own farms. I think of a story I read in the Washington Post recently about a Green County farmer who had a dairy, Brown Swiss herd, and he was struggling to make ends meet, had reduced his herd size considerably to make it a one-person operation to see if he could manage to continue farming in that capacity, but found that he was still struggling. And he was wondering if he needed to end his dairy, but what he ended up doing is he opened an Airbnb and he had people come stay at his farm and then experience the farm and really connect with Mother Nature themselves. So it was a really good way for him to continue farming and then share the joy of farming with others. I think that that’s just a unique way, and I know a lot of farmers are diversifying the way that they’re doing agriculture. It’s just one example of what people are doing, here.
So care farming allowed farmers in Europe to diversify their income and also increase their productivity.
And when we researched who started these care farms in Europe, we found that it was farms who had, farmers or farms that had spouses that worked in healthcare or maybe previously worked in healthcare. So they had the expertise in healthcare and they had the expertise in agriculture to make care farming work. As care farming gained support in Europe, there began to be a shift or migration to care farms starting in healthcare settings, starting in hospitals, such as the like VA hospital, here. And they would partner with farms in the community to provide this. This was likewise found to be successful in offering care farms and also beneficial to the farmer.
When studying the initial startups of care farms, those that had just solely agricultural experience and no healthcare backing or support, those care farms were much less successful. They just didn’t have that unique cross intersection between healthcare, human services, and agriculture, that made the care farming system so successful.
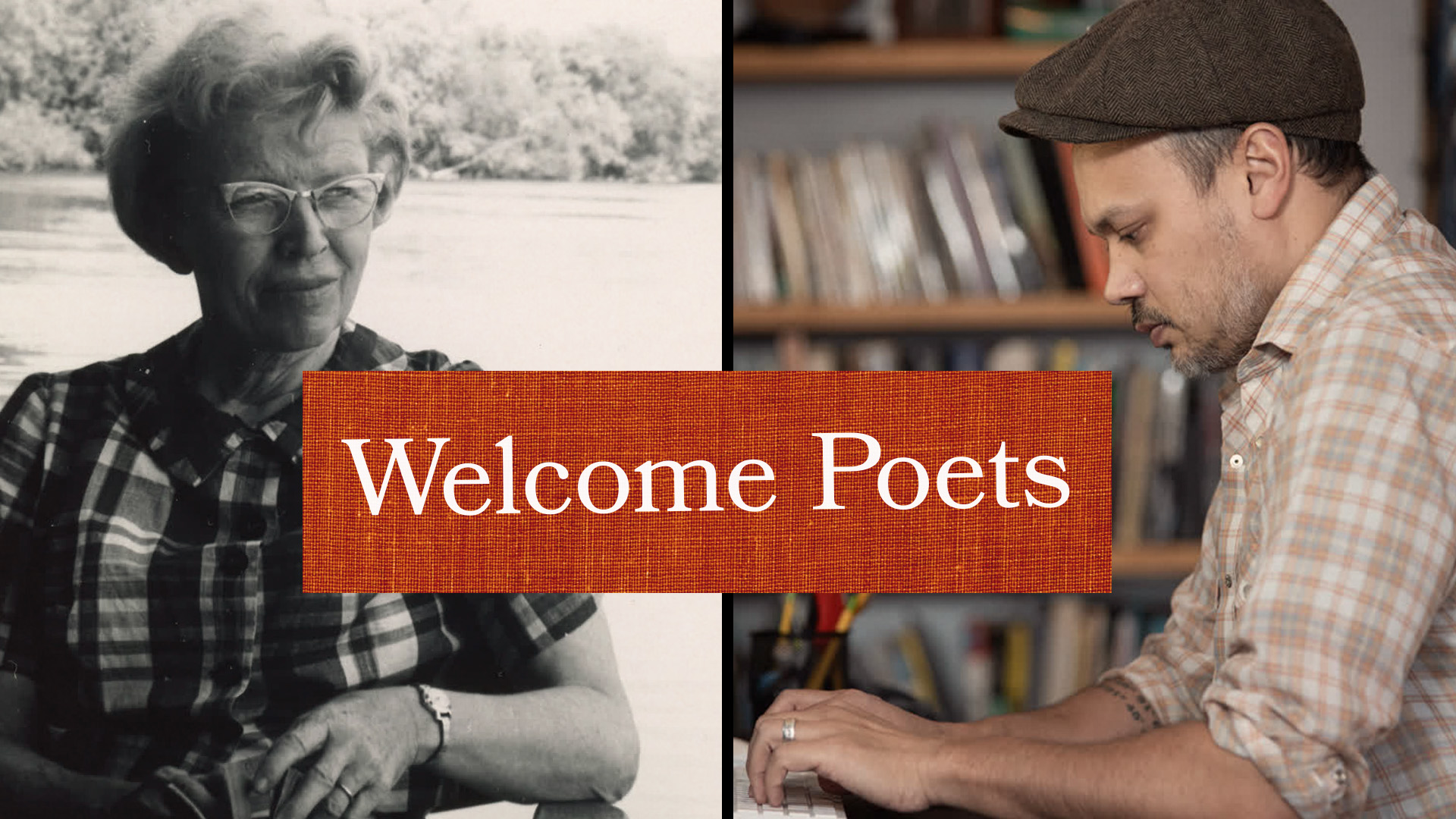
So care farming in the United States. Where we are today with care farming is that it isn’t traditionally funded by our healthcare system or supported by insurance. It’s typically funded through donations, private payments, grant funding. And it is less prevalent, but it is growing in popularity. We have locally seen an increase in community gardens. And, one that I wanted to highlight is Community Groundworks. That’s at Troy Gardens here in the Madison area. And they have a program that is specifically for veterans called Gardening For Good Veterans. This is a gardening program that allows veterans to learn about gardening and to self-direct their gardening experience, while socializing with other veterans who have a shared lived experience. So, I don’t want to talk too much about it cause I wanted to invite up an army veteran, Luke Cleaver, who’s been participating in Gardening For Good Veterans for about a year and a half now, and he’s going to share his experience with that program.- Hi.
My name is Luke Cleaver and I am part of the Gardening For Good Veterans Program like I was introduced. But, I think it needs, for me, I just want to tell you how I got to that point. So a couple of years ago I had a mental breakdown. I called the hotline like I was supposed to. I called the veterans hotline like I was supposed to. Three police squad cars showed up to my house in my neighborhood. My house is planted right in the middle of the neighborhood so everybody in my neighborhood saw that there were three squad cars that showed up to my house.
I got to the VA, the police took me to the VA.
They didn’t escort me, I got to ride in a squad car. Up front, I guess, but I did ride in a squad car. And I got to the VA and I talked to the nurses, and none of the nurses would help me without a police officer being in the room.
Then I got to talk to a couple of people who were interns, who were 22 years old, and they gave me a questionnaire. And I filled out a questionnaire.
And then, after I got done talking to the 22-year-olds, I got to go up to the second floor of the mental health facility of the VA. They locked the doors, locked both of the doors behind me, and that’s where I stayed for the night. Then, I met with somebody else who was 21, 22, and I filled out another questionnaire.
And the whole time I was there at the VA, everybody asked me what medication am I taking. I’m not taking any medication. And the look that the VA representative gets on their face when you tell them that you’re not taking any medication is priceless because the first thing that they want to give you is pills. I didn’t want pills. I wanted answers. I wanted to know why I had this breakdown and what it was all about. I wanted to talk to somebody, I wanted to talk to a doctor. So, behind the locked doors I got the opportunity to talk to a doctor. And I got an opportunity to talk to a doctor, the three 22-year-old interns that were sitting in the room with me. There was a county counselor and there was another doctor there, all looking at me, asking me what’s wrong with me.
So after talking to the doctor, talking to somebody who studies this sort of thing,
they decided that it was a breakdown and that I needed to go seek counseling. I needed to talk to a therapist, I needed to talk to the VA. So, they sent me on my way, again, asking me what kind of pills I needed to take with me.
So, my first initial experience with the VA was not a pleasant one.
It really kind of discouraged me from wanting to seek help. It made me more isolated, it made me rebel against my government, against my friends, against my family, and against the VA. It really made me upset.
And I really got a, “You can’t tell me what to do” attitude after that. I was looking for blame, I was blaming everybody. I’ve had, I had six different jobs at the time, because I would always tell my manager that, you know, this, that, or the other thing, you can’t tell me what to do.
Somehow, I found Gardening For Good Veterans. I’m not sure who I talked to. I’m not sure where it came about, but they pointed me in the direction. And I still had that rebellious attitude, I still needed that rebellious attitude, you know. “Ah, here’s some seeds, we’ll throw them over here, “we’ll throw them over there. “Weeds, whatever, we’ll pull weeds how I want to.”
And Marge and Jason and all the people who helped were like, “Yeah, yeah, go for it man. “Do you man, that’s exactly what you should be doing. “You’re a rebel, I’m a rebel, welcome to the rebel group.”
So I ended up, started pulling weeds, I pushed more dirt, I used some muscles, I did some wheelbarrowing, I dug some holes, I planted some stuff.
And then we would sit, eat some food, talk. Eat some food and talk with other veterans. The same people that went through the same thing that I went through. Or maybe not the same thing, but close to it. We had the experiences, and we could talk about it. And we ate food and we talked to each other and it was a great experience because the rest of my day I just felt better. I felt calmer, I felt more relaxed, I felt more open to suggestions, I felt more myself. I felt like a human being again.
So based off of that human experience,
there was a level of acceptance that came to me. After working it for a while, I figured I could plant whatever I want however I wanted to plant it.
It was my universe and I had control over it. I had control over my garden, I had control over my life. All I had to do was accept that there was a process that needed to happen.
So after a while I came back to the VA and started that process over again. I came back to the VA and I started filling out the paperwork and going to the doctors and talking to the counselors so that I can get my benefits and I can say and I can feel better about myself, so that I could participate in more things like this.
I accepted help.
Today, I have chickens, which is awesome. I don’t know if anybody here has chickens, but it’s a great experience. I have a peach tree. I’ve planted some blueberry plants and since they are recording this I want this on the record, just because you’re planting blueberry plants doesn’t mean that you guys are entitled to eat my blueberries. I want you guys all to know that.
But it empowered me into believing that anything could happen by taking the time to do it. I planted watermelons and even though two grew, I made those two grow. I helped make those two grow.
Right now, I’m not sure of my future. I’m not sure, but I do know that it’s okay to believe in myself and what I can do. And it’s okay to believe that there are people around me that want to help with that. And everything is a process and sometimes you just need to embrace the process. You can plant whatever you want, but you have to weed, you have to fertilize, you have to take the time to help those things grow. Just like human beings, we have to take the time to help each other grow. And that’s what I learned at Gardening For Good Veterans, that sometimes things just take time, sometimes things are a process, but you have to embrace that process and you have to accept that time that you put into it is the time that you get out of it. So I just want to leave, just for anybody out there, if you are suffering from anxiety, from depression, if you are a veteran, if anybody out there is a veteran and you’d like to join us, we meet Mondays, every Monday at 11 a.m. We’re also going to start meeting on Thursdays at 6 p.m.
If you’re not a veteran and you just want to come garden, Troy Gardens is a great place to do it. They’re good people, they’ll show you the ropes, they’ll show you everything that you want to know, and they’ll do it with a smile on their face because it doesn’t matter if you’re a rebel, it doesn’t matter if you’re a conformist, it doesn’t matter who you are as a person, they’ll show you that process to make you the best person that you can be.
So, yeah, so I think I’m going to just leave with that. Thank you for your time, thank you for listening. And Denise if you …
(audience applauding)
– Thank you so much, Luke. That was exactly how I think, how a lot of people do feel about their first experience with healthcare at VA. Or not, I mean it can feel that way and how trying different models of healthcare to empower veterans really is the right way to provide services and it’s something that the VA hospital is definitely adopting as our radical redesign, so thank you.
So, how did we get to this Pilot Program?
The Veteran Affairs Farms Pilot Program came about in 2018 there was a legislative directive that came from the Rural Healthcare Initiative and they directed the office, the VA Office of Rural Health to “create a pilot program to train veterans “in agricultural vocations “while also tending to behavioral and mental health “needs with behavioral healthcare services “and treatments from licensed providers.” There was a lot of stuff they wanted us to do here in this Pilot Program so I’m going to break it down just a little bit. The first thing is rural. They wanted veterans who are in rural areas to be able to access our healthcare in a more effective manner. The next part of it is agriculture. As we know, agriculture in America is struggling right now. The average age of a farmer today is over 58 years of age, which means that we have farmers who are in their 60’s, 70’s, 80’s, or even older who are still farming that may be ready to retire at some point and pass on their farming legacy. And at the same time younger people are not choosing to go into agricultural vocations. They have other options they may find more fitting or more financially lucrative. But for whatever reason younger generations are not as frequently choosing to take over those farms. The next part of it is the training component. As I mentioned, younger people are not going into it so you may be having individuals like Luke who didn’t necessarily grow up farming but has gained an interest in farming down the road and may have an interest in continuing to farm down the road.
But formal training and hands-on training is so important. You can’t just go out there and like Luke said, just start throwing around seeds and expect that everything is going to work out right. With time and patience you learn, and with proper training you learn the most effective ways to farm. The next part of this initiative is behavioral and mental health needs. Veterans are coming back to America after their service with significant mental health, and behavioral health, and physical challenges and struggling to reintegrate into society and struggling to reintegrate into work when their previous life and expectations that America gave them was to act a certain way and to behave a certain way and it’s very hard to reintegrate back into. So healthcare and services are so important for veterans to be able to connect with. And the last part of that is vocations. How this pilot program sets apart maybe the traditional care farm model is that we do want farmers to have younger people get into that vocation and veterans could be that route in which that could occur. So we do want vocational outcomes. So back in May 2018 the Office of Rural Health sent out a request for applications to all of the VAs around the nation asking us to submit applications to answer this very directive.
And we had two weeks to do this. So it was a pretty tall order to get that application put into the Office of Rural Health. But no surprise, I think to anybody in this room, that Wisconsin has a very strong, passionate agricultural community, and we immediately had support to get this going. A group of people from the VA who had backgrounds in agriculture and myself and then Steve Ventura from the UW-Madison Farm Industry short course, he’s a professor there, all got together and started thinking about what do we want to do and how do we want this to look. And we were able to put our application in with agents, with our VA leadership, we were able to meet the deadline and put our application in. And then we waited for a while. And in July 2018, we received word from the VA Office of Rural Health that we were one of 12 different, one of 12 sites around the nation, to have received this special purpose funding, and to do the VA Farms Pilot Program. So our vision is:
“Rural veterans will be empowered to improve “their health and well-being and thrive in their communities “through increased access to training opportunities “in agricultural fields, meaningful therapeutic work, “and Whole Health care.” And how are we going to do that?
So this is our mission, we want “to increase our support “for rural veterans who are re-entering “or entering the workforce in agricultural vocations “partnering with community organizations.” The partnering part is pretty big for us. We know we have a lot of support here. It’s making sure that people are aware that we are doing this, and we want to be a part of the community and support initiatives that are already in place that are helping veterans in agriculture and just everyone moving forward in the same direction. “To provide high quality education, training, “therapeutic interventions, on-the-job experiences “and Whole Health care with an emphasis on Mental Health. “This will revitalize interest “and entry into agricultural workforce “and empower Veterans in rural areas to thrive “through whole-health well-being.”
So when we put in our application to the Office of Rural Health, we really wanted to share with them why Wisconsin is so special and why we love agriculture here.
So, this is according to the USDA 2017 Wisconsin Agricultural Statistics report. Not surprising to anyone that Wisconsin ranks number one in all cheese production, but we also rank number one in dry whey, milk goats, mink pelts, corn silage, cranberries, ginseng, and snap beans. There may be some more but those were the ones that I came up with out of that report. And in the whole nation we’re number two in certified organic farms. We are a national leader in innovative production and marketing systems for fresh and value-added produce. The Department of Agriculture, Trade and Consumer Protection Program has launched an initiative to make sure we’re marketing Wisconsin and Wisconsin businesses, so you may see those labels that say, Something Special from Wisconsin. Or, if it’s a Veteran-owned Farm, Homegrown by Heroes. It’s just a good way for consumers to know that they’re purchasing something from Wisconsin, that is something local. You’ll see a lot of that in the market places, local from Wisconsin and what have you. I’ve never seen such an amazing support for small businesses as in Wisconsin. We really do a great job of making sure our small businesses have backing, I think. And then 10% of employment in our state is in agriculture and food processing. Now I believe that it would be much higher if we counted grocery stores and restaurants and hospitality and tourism that also uses local foods and everything, but as far as just strict employment in agriculture and food processing, it takes up 10% of our state employment.
And then, why is Dane County and the Madison VA hospital a good choice for this Pilot Program? We have a lot of agriculture in Dane County despite it being fairly urban because of Madison and Middleton and all the cities around the surrounding area. We are one of the largest producers for corn for grain, soybeans, milk production, and alfalfa in Wisconsin. We’re number three in Wisconsin for milk production. We’re following Fond du Lac and Clark Counties. We’re fourth in Wisconsin for counties for cattle. We have over 2,000 small farms in this area, a lot of them producing for local markets, and this gives us a lot of opportunities to do internships and on-the-job trainings for veteran farmers that are getting started. A great way to support them. We do host the largest farmers’ market in the nation, here in this capital, and we have 50 community-supported agricultural business operations in the area.
So our Pilot Program is pretty simple. There’s a lot going into it, but we really break it down to three processes. We have funding in our Pilot Program for formal training, to pay for formal training, to pay for placements, training placements, and of course our therapeutic support that is built-in.
For formal training, we decided to partner, for this Pilot Program, with two local educational institutions. The Farm and Industry Short Course at University of Wisconsin-Madison, their College of Agriculture and Life Sciences. And they have a one-year certificate program in foundations of farm management and then individuals can go on and do one of six different specialty areas. They have urban agriculture, meat and animal farm management, farm equipment operations, diversified agriculture operations, dairy farm management, and crop and soil management. I think they may have one more coming along, possibly organic farming. I’m not 100% sure on that. They also run their classes, so farmers continue to farm in like those heavy operation times so they don’t run a traditional semester schedule. They run a little off that so that they’re not interfering with farm operations as much. And then we also decided to partner with Madison College. The reason we did so is obviously they have a great agriculture program, but they also offer a lot of online classes and workshops which could be very helpful for veterans in rural settings that may already be farming and aren’t interested in coming into Madison for classes or aren’t able to just because they already have family themselves and are running their businesses. So at Madison College they have a one semester agriculture systems management certificate and then they also have a one-year certificate in sustainable farm-to-table modern meat production.
And our funding does pay for those, tuition for both of those programs, both of those schools and programs. And we don’t require the veterans to use their GI Bill, their Forever GI Bill to do that. Especially at Madison College, those are not, some of them might not be credit-based so there wouldn’t otherwise be funding for it, but our Pilot Program does fund that.
Okay. So the training placement, that’s kind of my bread and butter, ’cause that’s what we do at Compensated Work Therapy is we help Veterans get back into work. So how we do that is we partner with businesses in the community to provide the training. We make sure that the environment is safe and that they’re getting quality training and that it’s an effective training experience. Again, we haven’t focused in the past in agriculture so we will be setting up and have started to set up agreements with farms to provide training placements for veterans. We’re also, have started working a lot with Fairshare CSA Coalition and Department of Agriculture Trade and Consumer Protection Program for marketing outreach opportunities and some of you may be familiar with the Dairy Grazing Apprenticeship Program that started in Wisconsin.
We know that they’re in several states now. I think maybe six, I could be wrong, but they’re really expanding and do a phenomenal job of offering apprenticeships for those interested in going into dairy grazing.
So we know if a veteran is interested in going into that, we may be able to provide the formal training and then they could do an apprenticeship with the Dairy Grazing Program.
That program does also have an initiative to help veterans get into farming as well. So we’re excited to be able to partner with them.
The last part of our process is where we start to weave into this our Whole Health care and how that’s not a traditional model of healthcare.
Our goal with this VA Farms is really to empower Veterans to take control of their own healthcare. And it is really the initiative of the whole VA, but we really wanted to embrace that level and nature of care in our VA farms. The other icon I put up there is with AgrAbility. We do have a partnership and working relationship with AgrAbility. They’re a fantastic program that assists farmers to continue farming as long as they want to. Perhaps the farmer has a sudden accident or injury that makes it difficult to continue to farm at the same level they were before. Maybe a progressive condition that’s making it more challenging, or maybe it’s their spouse that has this condition and she’s been the one that really makes things work. And so without her, the farm doesn’t work. But they go out to the farms and assess the farms, do an evaluation and help the farmer come up with strategies, assistive technology and what have you so they can continue farming independently. But we hope that we will utilize their services for veterans getting into farming, because they too have barriers to employment when they get on site.
And the last part of that is really each veteran will be paired up with a health coach to develop a personal health plan that’s more than just what medication are you taking and what counseling classes are you taking, but really looks at the Whole Health model of care for services.
So what is this Whole Health care? It really focuses on preventing mental health, preventing health problems, by giving people the awareness of what matters to them, the tools to live a healthy lifestyle, and make the changes that they want to make.
This slide is kind of a fun one to look at. It’s a slide that shows life expectancy in the vertical blue lines going up and down, and then the purple line weaving across it is expense, healthcare expense per capita. And you can see, Japan is our highest one as far as life expectancy, way up there, and their cost of healthcare is pretty low.
The United States has that really big peak in cost to the right of the graph and it is– The cost of healthcare is nearly double that of any of the other nations here and yet our life expectancy is the same as Cuba. And you can see that Cuba spends much less on their healthcare.
So our expense does not seem to be giving us sufficient value and return on our investment. This slide was given to us by the University of California Santa Cruz Institute for the Future. Another slide that demonstrates how we’re spending our time and our energy in our lives and what really contributes to our whole health is not our clinical care. So our clinical care is over here in the orange. Here’s my little– That’s 10% of our what we spend in time and energy.
The things that matter are social and economic factors, that’s things like our friends, our family, and our jobs.
That’s 40%. And then the other part is our health behaviors: eating, sleeping, and exercising, those lifestyle choices that we make. So, again, clinical care only makes about 10% of that, so are we really getting the best bang for our buck in terms of how we spend our time and energy in healthcare? Or is there a better way to do it?
So the shift, and I think Luke said it really well when he was at the VA the first time around was, there was a lot of questioning of, “What’s the matter with you?” But the shift in the whole health model is really, “What matters to you?”
We do know that individuals know what’s best for themselves, that’s true. Healthcare providers may have a lot of expertise, but we really don’t know what’s best for each individual. I wanted to share a little story about somebody that’s near and dear to me that had kind of this experience where he felt like the healthcare provider didn’t listen them. This wasn’t at the VA hospital, it was with a different provider, but it could happen anywhere. So this gentleman has a condition that causes his muscles to progressively weaken and he has a harder time walking and getting around and lifting things. He’s to the point now where he uses a wheelchair sometimes to get around, just for increased mobility, but he does want to continue walking. That’s really important to him that he has the ability. He takes a lot of pride in his ability to continue to walk. So he went to a physical therapist to ask for some stretching, some stretching exercises and maybe some toning ’cause he was having a lot of contractions in his muscles and having a hard time getting the range of motion that he needed to continue walking. And so he sat down with the provider and she was asking some questions and found out that he was falling sometimes when he was walking, and she became greatly concerned with the fact that he was falling and really felt that that should be the focus of his care, for him to not fall anymore. And he spoke up and said, “This is really an unrealistic goal for me “because my goal is not to not fall. “My goal is to continue walking. “And to continue walking means that I might fall sometimes. “And that’s okay with me as long as I continue walking.” I think it just goes to show that we need to listen and we need to ask the right questions in healthcare to make sure that we’re really understanding what’s important to that person.
So the Whole Health system has three different things that make up how we go about it with the VA. So, it is an approach to healthcare that empowers and equips people to take change in their health and wellbeing and live their lives to the fullest. So the pathways part of this, is up here, is creating personal health plans to discover the person’s mission. The well-being portion of this is, gives people tools so they can manage their own healthcare. They may have known that they have a condition but not really know what are some good ways, non-medical ways, that they could manage it or even prevent it from occurring in the first place. And then the last portion of this is the Whole Health clinical care. We do have a really strong clinical care in Whole Health right now, and they’re using treatments that’s driven by veterans’ choice to manage their healthcare concerns. And they’re using non-traditional treatment modalities: meditation, relaxation, mindfulness, tai chi, yoga,
acupuncture, all of those things that you wouldn’t traditionally see in VAs in the past.
As I talk about this slide, I just want you to think about a question in your mind, “What piece of this circle is a strength for you?” ‘Cause we all have different strengths.
No two peoples are like another, and you can have many strengths, but just think about which one of these is a strength for you. So there’s eight different components that make up our self-care. These are things that we can control in our lives to take care of our own, our own selves. So the first one up there, it’s kind of at the top, so I’ll go clockwise starting at the top, is working your body.
Getting out, exercising, getting some fresh air. The next one in there is your surroundings, either your physical surroundings or your emotional surroundings. That could include the places that you work, the home that you live in, your community, and the people that you are surrounded by.
The next part of this is personal development. This is your work and this is your personal life. I put in this one a lot of hobbies ’cause people do a lot of things that they do for self-care. Maybe it is playing the guitar or gardening or other things that you do to make sure you’re working your mind and taking care of yourself that way. The next circle down is food and drink, what are we doing to nourish our bodies? The one at 6 o’clock, at the bottom, is recharge: your ability to manage your sleeping and relaxation and are we getting enough of that? The next one is our family, friends, and coworkers. This is the social aspect, the people that we choose to be around with and other relationships that we have with those people. The next thing is spirit and soul. That could be a religion that you’re a part of or it could just be a spiritual, soulful involvement. And then the last one is power of mind. This is the internal dialogue that we tell to ourselves, our ability to control our thoughts and to use things like meditation or mindfulness to relax and take control of our situations.
So the next few slides, they’re just some examples of what health could look like for people. This is just somebody’s work station, this is their surroundings. They chose to use lots of natural lighting and plants to make their surroundings as good as possible. I mean if you’re working at a desk all day, you might as well enjoy what’s around you. The next thing is, this would fall under food and drink. Are we eating nutritious, whole health foods that nourish our body? The next thing is– This is actually a picture of my brother and one of my kids and two of his kids, but it’s just an example of getting out, exercising, having fun, enjoying the little things, and how much time do we spend doing that or are we rush, rush, rushing around and not taking time with family and getting out and relaxing.
I love this slide. This is just an example of a modern-day Christmas dinner. And it’s just an example again, of nourishing your body, but most importantly socializing with others, sitting down and having a meal together, laughing, connecting, and breaking bread together.
Probably my favorite thing to do is napping, so I put this one in there. But it’s very important that we unplug at times. That we slow down, we go outside, relax. We make sure that we are getting plenty of rest in our day. But these are just all examples of Whole Health and things that we take control of in our daily life. There’s no prescriber telling us that you have to do this. This is stuff that we can do in our own environments to have a more, whole lifestyle.
So bringing it all together, I’ve talked about quite a bit today, but really all of the things really relate back to our VA Farms pilot program with our involvement in education, getting veterans back into agriculture through training, hands-on agriculture experiences, and then the Whole Health care model of healthcare.
So how would someone get started and how could somebody help?
So I am, again, the therapeutic and support employment services program manager and I am the supervisor, kind of the cat wrangler of this VA Farms Pilot Program. My contact information is on there. As far as veterans, one would just need to be a patient at the VA hospital to be at least eligible, would need to be a patient and then get in touch with our program. If a farmer was interested in maybe hosting a site or being part of our advisory council, we do have an advisory council made up of farmers and local agriculture business that are helping us make sure we’re running our operation as best we can. They too can get a hold of me and I can help them out, connect them with the right people, and see if they might want to host veterans on their farm.
Okay this is my last slide. I want to thank everybody for coming out today and listening. This was early in the morning to listen to something not super duper exciting, but I hope you took away a lot from this. I want to think the VA Farms Advisory Council, could not have done this without the VA Farms Advisory Council. We really value their first-hand expertise. I want to think Luke Cleaver for coming out and presenting so well with me and really sharing his experience with us. Thank you to UW-Madison and Madison College. To my co-workers at the VA.
For Roxanne Wankeys for helping me with this PowerPoint, she’s fantastic. And then VA leadership for supporting the VA Farms Pilot Program so we could get this started in Madison and our goal is to keep it going for years to come. Thank you.
(audience applauding)
Search University Place Episodes
Related Stories from PBS Wisconsin's Blog

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport

















Follow Us