– Good evening. Welcome to Mini Med School. I’m Rebecca Minter, I’m one of the Mini deans that’s thrilled to be here this evening. And before we get started, we wanna give a big shout out to our alumni who are here with us from, many coming from far away who are here for Alumni Weekend. So thank you for being here with us. And we hope this will be reminiscent of your time here as medical students. We have a record turnout tonight. I think this is the largest number of people we’ve ever had at Mini Med. There are 668 people here this evening. [audience applauding and cheering] Filling three auditoriums and it’s obviously a testament to the importance of the topic and the wonderful speakers that we have here tonight.
But we also are really fortunate at UW and in Madison to have really fantastic resources around fall prevention. And so, thank you for being here. And I will turn things over to Dr. Rice. [audience applauding] – Good evening, we’re so glad you’re here and we do have a great program for you this evening. Now, it’s my great pleasure to introduce our emcee this evening, Dr. Betsy Trowbridge. She is the Interim Chair of Internal Medicine and the Philip August and Sarah Herrmann professor here in the department. She did her residency in medical school here, she’s all Wisconsin, and we are very fortunate to keep her on the faculty all these years. She is pretty close to singularly responsible for the transformation of our Primary Care Unit in the last 10 years, and has just done a beautiful job and continues to do so.
She’s a graduate of a very prestigious women’s leadership program at Drexel University, ELAM. And she is the Helen Dickie Award– received the Helen Dickie Award for Outstanding Woman Physician for the American College of Surgeons. She’s on the UW Authority Board, and more importantly, she’s on the Green Bay Packer Boards. Come on up here, Betsy. [audience laughing and applauding]
– Thanks for that handoff. So I was gonna do a pratfall up here. But I tried it in the hallway and it was a disaster. So I’m not gonna pretend to fall. We are so excited to have all of you here tonight. With this Mini Med about falls.
I think you’re gonna walk away from tonight with a lot of knowledge about falls, some practical ways to prevent falls, and you’re gonna learn about some very exciting programs that we have here at University of Wisconsin, that can really make you and your family more safe. We have four incredibly fantastic expert speakers tonight, and I’m just gonna tell you a little quick blurb about them before I go in more detail later. Our first speaker is a trauma surgeon here who deals on an everyday basis with people who fall and have complications from falls. Our second speaker is a physical therapist who works in rehabilitative neurology, and works with patients who have disorders that put them at risk for falls everyday, and is gonna talk to us about some practical knowledge that she has about preventing falls. Our third speaker is a emergency room physician and geriatric physician who works in a clinic called the Faint and Fall Clinic, which is quite a unique clinic here at University of Wisconsin, that diagnoses people, like many of us, who might be in this audience, who are falling for reasons that can’t be understood. And our final speaker is a researcher who is a geriatrician physician, who has spent her life studying geriatric issues and really very specifically, falls and has done some incredibly innovative work in finding out and studying the science behind falls, and really telling us what does really work and does not really work. So all of us fall, people who are famous fall, people are not famous fall. When I think about falling, and I think about my life and looking at the news, I remember Ronald Reagan fell off of his horse. And when he fell off of his horse, he had bleeding in his brain. And then I think I grew up in Green Bay, I’m on the Packer Board.
Max McGee, a beloved Packer, had a horrible fall, a few years ago, he was on his roof. And I tell all my patients, if you’re over 40, four steps up, that’s it. But he was much higher than that, he fell off of his roof and actually died. And then, you know, most recently, you might have all read that President Carter fell and broke his hip. And these are all very serious events. But it is not just older people that fall. So when I was looking through people who fell, my partner was like “You have to have a woman who fell. ” So Beyonce fell during a concert on her dress, walking upstairs, multitasking, right straight down on her face, and thankfully wasn’t injured. So, all of us have a risk of falling. So why am I the emcee, and why am I here? So I’m a primary care doc.
I’m a general internal medicine doc. And I care about falls because my patients fall, and sometimes they’re injured, sometimes they’ve had complications where they’ve actually passed away. And many of my patients are just simply afraid of falling and need to know what to do to mitigate that risk. And those of you who have primary care physicians at UW Health, you might know, we care so much about falls here at UW, that if you’re over 65, you will be screened for falling at UW Health once every year and given literature about how to help you to not fall. So, I’ve learned a lot, I’ve seen this lecture twice. And I’ve learned a couple things. One of the things I’m gonna do to mitigate falls, which I started already is this, I walk and talk on my phone, I watched my steps on my Fitbit as I’m walking down stairs, I’ve learned how dangerous that is. And I’m gonna stop that. And so you’ll learn some of the things you can do to stop your risk of falling. You’ll also learn what you have to do when you just have things in your life that put you at risk of falling and that you don’t wanna change, and I’m gonna show you those two things in my life.
So I have puppies, so Wally is that poodle and he’s a pet pal at the Children’s Hospital. And Sammy is the little white Bichon and she is deaf and blind and 15, and I’ve fallen over her more than once. And my other risk of falling that I’m not giving up is Melvin. And Melvin is bigger than the Bichon. (audience laughing) So, I’m hoping that you’ll learn just a few tips and tricks to make your life safer. And with that, we’re gonna start with our first speaker. So Dr. Ann O’Rourke, MD, PhD, is the Trauma Medical Director here at University of Wisconsin. And you may not know this, but we are a level one trauma center here, one of two in the state of Wisconsin. She is an associate professor of surgery here.
She’s been part of the Peace Corps. She did her MD and PhD, both here at University of Wisconsin. She also completed her surgical residency here. She then went away for fellowship, she went to Memphis for her trauma and surgical critical care fellowship. And like Dr. Rice said about me, we are very lucky to have Dr. O’Rourke come back and join us here at University of Wisconsin. She’s very involved in education as well. And she’s the Director of The Medical Student Surgical Education here at UW. And something not on your little agenda, she just received the Dean’s Teaching Award, one of the most coveted awards here at the School of Medicine and Public Health in 2017.
She serves on the board of directors for the World Association for Disaster and Emergency Medicine. And she just has a fantastic talk. So Dr. O’Rourke, come on up. [audience applauding]
– Thanks so much. Thanks for that very nice introduction. I also will try to keep to the right of the tape. Thank you all so much for coming. As a trauma surgeon, I think people have ideas that we like to consider ourselves like the rock stars of surgery. But I would say the most common problem that I care for daily on my trauma service is patients who’ve been injured with falls.
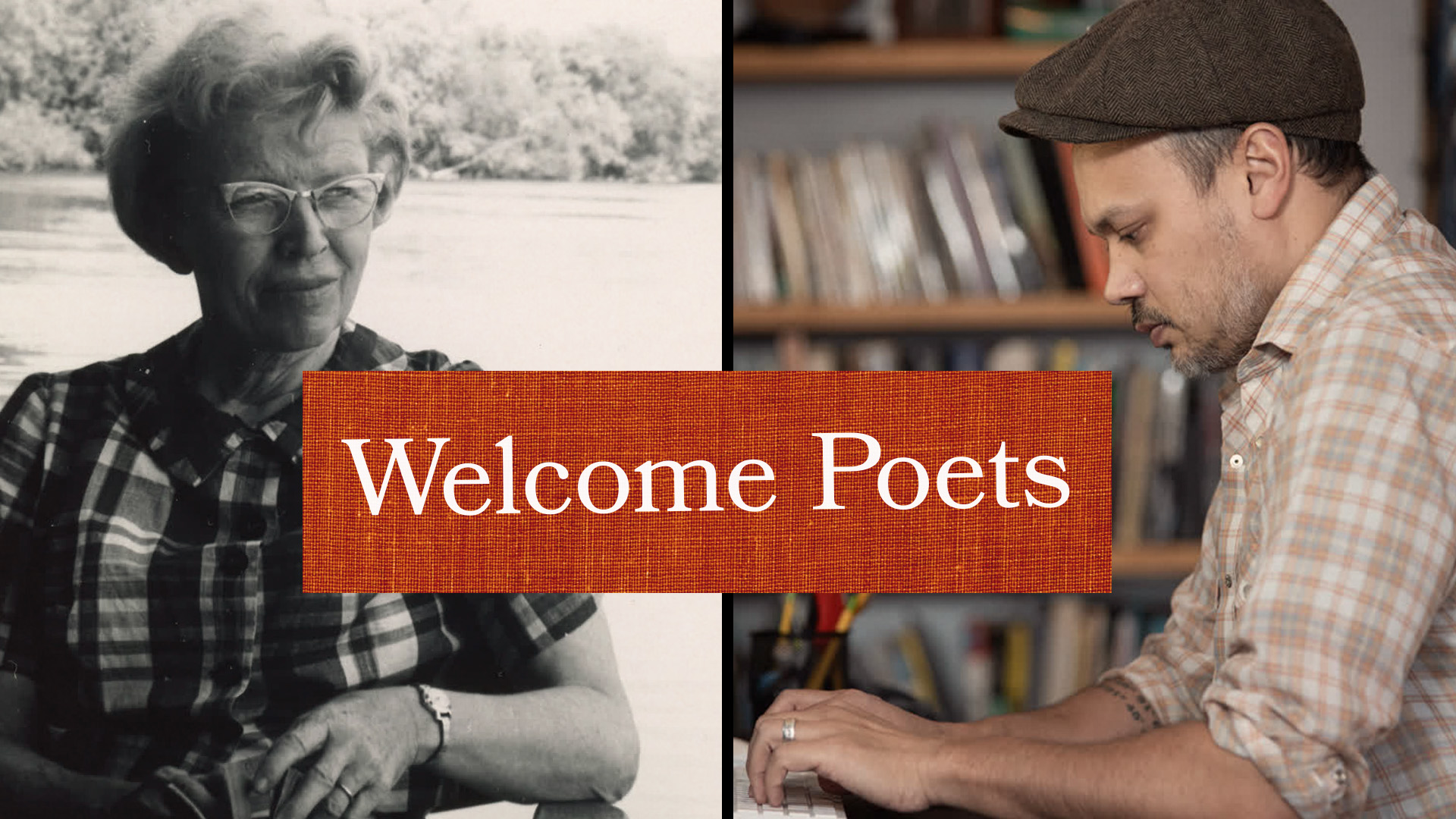
And I just wanted to share one of the reasons this is so important to me personally, this is my grandmother, Ethelene Crowder Womack, which is the most Southern name you could ever come up with. I’m from Tennessee originally. And she broke her hip not once, but twice. And when I was in college, was the first time she broke her hip, and I had all these devastating horror stories about “nobody does well after they break their hip. ” And I just wanna leave that up there. This is after she broke her hip. And she always told me that she didn’t care what I did in life, I could dig ditches, as long as I had a good education because I would be happy in my mind. And so she was a very much an inspiration for me to complete my education. So that’s my inspiration for tonight. And really, I’ve been asked to set the stage Why– I mean, clearly we have such a big audience.
I think we all know that this is important. And it’s something we worry about, but I just would like to kind of talk about the problem of falls in general. And what we really know is that falls are very common among older adults. One in four people over the age of 65 will fall each year. One in four. Even for me who has a master’s in public health, that is a stunning statistic. It’s very costly to our health care system. But these things are preventable, and the rest of tonight I think will be, after I sort of have been sent up here to be the heavy and talk about what a big problem it is, we’ll talk about how we can keep this from happening. Over three million people are seen in the emergency department each year, and almost one million of those are hospitalized, and that’s where I come in. In falls and patients over 65, one in five of those falls result in serious injury.
And by serious injury, I mean things like broken bones such as broken hips, or broken ribs, or bleeding in the brain. The death rates from falls are continuing to go up in our country, despite the fact that we know and the Centers for Disease Control know that this is a serious problem, fatality due to falls continues to go up. Here in Wisconsin, in year 2017, eleven and a half thousand people over 65 were admitted to the hospital for a fall. That’s just here in the state of Wisconsin. And of those eleven and a half thousand people, 69% of those people went to a nursing home, after that hospitalization for the fall. 25% of them went home, and of those patients who went home, the majority of them went home with some needing some extra help, such as home health or ongoing physical therapy. And 6% of those patients who were admitted for falls did not survive. About half of those progressed into palliative care or hospice, but half of them, 3%, did not survive their injuries. So here in Wisconsin, it is a problem. I wanted to talk about the common injuries that I mentioned, the serious injuries that we see, and the consequences in those.
A hip fracture I think is the thing that I think many people are very afraid will happen. And my grandmother was one of those people. Of patients who break their hip, 20% of them die within a year of their injuries. 30% of them go on to have some sort of permanent disability. 40% of them are unable to walk independently. And 80% of patients who break their hips, need some additional help with their activities of daily living. Some part of their life, they’re not able to do independently any longer. Which I think is something most people in this room already know, and why it’s so frightening. These are the injuries though, that I think people don’t take as seriously. And I spend a lot of time actually in my role as a trauma medical director, going to other trauma centers in the state and talking about broken ribs.
I think when we hear the thing like broken ribs, “Ah, I just broke a couple of ribs, it’s not a big deal. ” I’m here to tell you broken ribs are a huge deal. They’re a big problem; in our patients who are over 65 years old with three or four broken ribs, one in five of those people will die from those injuries. And one in three, will develop a pneumonia. If you have greater than six broken ribs, one in three of those patients will die, and half of them get pneumonia. When my patients are in the hospital with broken ribs, I come in and I meet them and we have a little chat about how I am not their friend right now, I am their coach, and it hurts to cough and it hurts to take a deep breath. But we’re gonna do that anyway because we wanna keep people from getting pneumonia. Our whole Intermediate Care Unit on our trauma ward, we built in mind for patients with broken ribs to try to prevent them from getting pneumonia. And the other common injury I wanted to speak about is brain injury, bleeding in the brain. Many patients, many of you probably in this room need to take a blood thinner because of other health problems that you have.
What bleeding in the brain, I think we all understand maybe has some hot mortality associated with that. But the other things that our patients with brain injuries will tell us about, is that after their injury, even after they’re ready to go home, they had some sort of cognitive impairment; their memory is not as good, they’re not able to multitask as well. Patients also have some other lingering symptoms such as emotional problems, particularly depression. Dizziness, which feeds into possibly another fall, and sleep problems. The good news though is, is that rehab is slower than if you were younger with a brain injury, but real gains can be made. So a brain injury is not a hopeless situation, it just might take a little bit longer for those symptoms to go away. Trauma centers like ours and others, patients who are elderly and who fall are actually less likely to be referred to a trauma center. I think we still think falling down, breaking a couple of ribs is not really a big deal. But a third of patients, you’d be a third less likely to die if you presented to a trauma center with your injuries after a fall. And here at UW, our level one trauma center has compared to our peers in nationwide institutions, have better outcomes in our injured patients, our elderly trauma patients than other trauma centers that we’re compared with.
I just wanted to finish up actually with my grandmother again, I love this picture of her. My eyes are closed, it’s fine. But as I said, she broke her hip not once but twice. She broke her wrist and she had several compression fractures in her spine. Bone health is something I take very seriously for myself. She, after she broke her hip, was fiercely fighting for her independence, and insisted on returning home and doing her own rehab. And her rehab included goin’ to the Walmart everyday and walking and going to the fabric department and hanging out with her friends. But before she could go talk to all her friends in the fabric department, she would do a couple of laps around the Walmart with her walker, and then she graduated to a cane and then nothing. And then several years later, she broke the same hip, had a fracture around the prosthetic hip she had in place, and she did the same thing. She’s the strongest person I know.
So even with two broken hips, broken wrist, a few compression fractures, my grandmother lived independently until she died in her late 90s. And so, these injuries are serious, but they are absolutely recoverable with help. And with a fighting spirit like Ethelene Crowder Womack. Thank you. [audience applauding]
– Betsy: Awesome. Thank you. Is this on? Yeah, nope, yes. Thank you, that was fantastic. I think those rib fractures statistics are just mind-blowing. And I think that take-home message about you’re never too old to ask for the right care like a level one trauma center is great.
Our next speaker, Dr. Laura Guse who actually is a doctor, but she said physical therapists don’t necessarily like to be called doctors, is a physical therapist. She has received her doctorate in physical therapy here from University of Wisconsin. And she is the person who has that specialty area, she practices in our UW Health Rehabilitation Clinic, and the kind of patients that she takes care of are neuro rehabilitation patients. They’re patients who have complex neurological disorders like Parkinson’s disease, strokes, traumatic brain injury, and right up our alley, she deals with people who have had balance problems and inner ear problems, another huge risk for falls. She’s a member of the American Physical Therapy Association in the Academy of Neurological Physical Therapy, and is a board-certified Neurological Clinical Specialist. And this is the kind of person you really want on your team if you are having trouble with fall. So Laura, come on up. [audience applauding]
– Thank you. Can everybody hear me okay? Very good.
I have been a physical therapist for eight years. This is a second career for me. And I’m so glad that I made the change. Because this is a job that I feel a lot of passion for helping people to get back to a higher level of function and reduce their risk for falls, so they can go out and do the things that they enjoy doing. I’m here today to talk to you about risk factors and mechanisms for falling. So, I think Dr. O’Rourke made it pretty clear that falls are bad. This is a huge issue for us. And you have to wonder why hasn’t this been solved yet? It’s just a fall. Well, the fact is, this issue is really very complicated.
There are a lot of risk factors. But if I leave you with nothing else today, I want you to consider that there is hope for us to work on solving this problem and actually make gains, and making this a better situation for us. So, let’s delve right into the risk factors. First, let’s talk about risk factors that we can’t change. So if you’re over 80 years old, you have an increased risk for falling. Obviously, no one has figured out how to change aging. So we’re stuck with that one. People who have neurological problems such as a history of a stroke, or Parkinson’s disease, or multiple sclerosis, also at a higher risk for falling. People who have cardiac issues, arthritis, impaired thinking, history of falls, these are all things we really don’t have a lot of control over. But let’s talk about the things that we can change.
So, I don’t advise doing this on your own. But with help from your physician, you could maybe have your medications looked at or solve depression, or change your glasses, or something to improve your vision so that these things could reduce your risk for falling. But only with the help of a physician, as I said. Now, here are some things that a physical therapist can help with: walking and balance problems, weakness, talking about the proper footwear to wear in summer and winter, and working on your environment. Now, I don’t expect you to have all of those risk factors memorized already, although this is Mini Med School. (audience laughing) But I would like you to think about this in terms of this triangle, of the individual, which is you and me and the characteristics of our bodies and minds. Also the second point in the triangle, the task, what are you doing? And the third point of that triangle is the environment and challenging features that might be in the environment. So first, let’s talk about the task. I have worked with people who have fallen getting out of bed. I have worked with people who’ve fallen standing up and trying to sit down.
I have worked with people who have fallen on the stairs, I have worked with people who have fallen while they’re walking either by themself or with a dog who might have nudged them a little bit and pulled them right over. These are things that most of us do just about every day. This is the picture of the environment. Now you might know that– (audience laughing) (muffled talking) What is so funny? Does this look like your house? (audience laughing) So, I think a lot of people logically know that going up a ladder has hazards, that is a difficult environment and a difficult task. And being on a roof is a very difficult environment, especially if it’s the middle of winter, and you’re scraping your snow off of the roof. But something that we should consider also is the hazards that are available to us in our own home. So, here is a typical living room possibly. I’m gonna draw your attention to the cane on the floor. Now a cane is a very good device for many people to use to help them walk better and lower their risk for falling. But a lot of times people will set it on a table, it’ll tip over, they’ll forget about it, they’ll step on it, and they’ll fall right on their own cane.
I want you also to notice this table has some corners that sort of jut out, and it’s kind of placed in the middle of the furniture in such a way that there’s not a lot of room to maneuver between those items. So trying to squeeze between those areas might also be challenging. The throw rug, many of us have heard that throw rugs are a hazard; very easy to catch your toe on when you’re trying to walk across the floor. And then other things laying on the floor; newspaper, shoes. Here’s another pretty common environment, a bathroom. And so on the picture on the left we’ll take note of this drawer that’s sticking out, someone could catch their hip on it. Another throw rug, more shoes, a trash can. So, when we look at the picture on the right, not only have all those hazards been removed, but I’d like to point out that in this slide, you can see that things have been added to help make this space even more safe, such as the grab bar that’s on the wall. The hardware around the toilet, we call it a toilet safety frame that can help someone stand up from the toilet and then they can grab the grab bar to stabilize themselves. There’s also a chair inside the tub so the person can sit down while they’re showering so they don’t have to worry as much about falling.
And there’s a handle to help them get over the tub so they can hold on to something while they’re trying to step into the tub. Finally, we get to the individual, and I think this is where a physical therapist probably offers the most value in terms of these three conditions: task, environment, individual. So, if you are referred to physical therapy to try to lower your risk for falling, a physical therapist would most likely look at the sensory system that you use for balance. There are three primary senses that we use for balance. First one is vision, what you’re seeing through your eyes, helps you orient yourself to where you are, so it helps with your balance. What you’re feeling through your body and your feet, your somatosensory system, in other words, is another key part of the sensory system that we use for balance. And the third one is the vestibular system which is found in the inner ear. So a physical therapist will look at how these items are working together, and how our brain is organizing that information to figure out if we need to work on that aspect. But the bad news is as we are aging, our senses can change. Our vision can become impaired, many of us are wearing glasses as we start to get older.
Somatosensory system may become impaired. So what you’re feeling through your feet may be muted, or distorted by conditions like diabetes, for example. The vestibular system might also become impaired. In fact, there’s literature to show that as we age, all of these things start to decline. A physical therapist, in addition to the sensory systems, will also take a look at the muscles in someone who comes to us to reduce their risk for falling. So, are the muscles flexible enough? For example, does a person have enough range of motion at their ankle to be able to pull their toes up sufficiently so that they’re not catching their toes when they’re walking down the street? Or how about the muscle strength? So if someone does lose their balance, do they have enough strength to brace themselves, so that they don’t go down? And finally, muscle control and timing. So, those are very key things for balance, can you respond quickly enough to keep yourself from falling? And just as with our sensory systems, our muscle characteristics also decline as we age. A lot of us just become more sedentary because we’re not running around with our kids anymore, taking them to 12 events in a week. So, because we’re maybe sitting around more, our muscles can get tighter, they can get weaker. And we might just be slowing down our timing and control just, things slow down.
Another thing that a physical therapist is going to look at is specialized balance tests and gait speed. We can tell a lot about a person’s balance by the speed that they’re walking. And we also have a lot of standardized tests that we do that have been given to many, many people. And they’ve been able to determine cutoff scores for those. So, a physical therapist might test you using some of those tests, look at your score, compare you to the other people who got a similar score, to determine very objectively if you are considered an increased risk for falling or not. And the results of these balance tests can help us drive treatment. So instead of doing an across the board standardized program for everybody, we can look at the specific characteristics of each individual and really focus heavily on the things that they need the most practice and work in. These are some other things that a PT is going to consider are those other risk factors that we talked about. Age, medications, impaired thinking, history of falls, history of other medical conditions, and smart choices. For example, I might talk to this lady about possibly considering more sensible shoes.
[audience laughing] I would ask her to not wear her reading glasses while she’s walking around. And I would encourage her to not put so much stuff in her purse that it makes her tip over. So a physical therapist is going take all that information and put it together to create an assessment and a plan. Again, I’m gonna look at the individual, the tasks that they are doing, the environments that they’re doing them in, and then figure out what I can modify, what can I work with this patient to modify, to lower their risk for falling. And I will, with the patient, create a plan, which likely will include a home exercise program. Specific PT interventions typically include, strength training, balance training, of course, in a way that is safe, we don’t want people to fall while they’re doing their exercises to train their balance. Often, we also discuss modifications to the environment and maybe changing some habits, which we’ve already touched on. And finally, I’m gonna just emphasize that if your physician refers you to a physical therapist to help work on your balance and lower your risk for falls, indeed, it is a partnership between the therapist and the patient. I don’t have a magic pill to give you that’s gonna make this better. I will give you suggestions and coaching.
And the real rehab and fix for this is gonna be you implementing some of these changes at home, coming back week after week for more sessions to progress your exercise program and lower your risk for falling, and ultimately discharge you at a reduced risk for falling. So, if you find yourself having balance issues, and you’d like to make that better, there is hope. And I would encourage you to contact your physician for a referral to balance physical therapy. [audience applauding] Thank you.
– So, Laura, thanks, that was fantastic. So for every talk, I’m gonna have one little pearl and I’d say that picture of the living room was awesome. And and my pearl is pick something from that picture that you do in your house that you can change. My household, it’s shoes. So, actually after we saw this talk, I have baskets in each room now and all shoes get thrown in the basket, which has been super helpful. So our next speaker is Dr.
Kathleen Walsh. Dr. Walsh is a clinical associate professor in the Department of Emergency Medicine. And I think Dr. Walsh, you have a joint appointment in medicine, I hope actually. She is the Associate Director of the University of Wisconsin Cardiovascular Faint and Fall Clinic, which is a fantastic resource for all of you in this room. She’s done two residences. She completed her first residency, Internal Medicine, here at University of Wisconsin. Then she went out to UCLA and she did her fellowship in Geriatric Research, and then, a glutton for punishment, she came back and did a second residency in Emergency Medicine here at University of Wisconsin. And again, we were able to have her stay here with us, which I think has been fantastic.
So she is a co-director of the Faint and Fall Clinic. And in that clinic, she works very closely, she and her colleagues, with people like me, who is a primary care doctor, doctors in the emergency department, and inpatient doctors to be sure that we are evaluating and managing patients who have recurrent falls, and fainting spells with falls, and helps us to diagnose those people. I also wanna say that this year, she was awarded the Lecturer of the Year in 2019, for the UW Physician’s Assistant Program, which is also a great honor. So Dr. Walsh, please come on up. [audience applauding] Take it away.
– Am I on? Good, good, good, good. Now, I am not a believer in bifocals or progressive lens. And I’ll let you know why in just a little bit. So I have to figure out which glasses I’m gonna wear here.
So, [audience laughing] let’s see, hold on here. I think, oh boy, I don’t know. [audience laughing] I’m good here, okay. All right. Oh, I can’t see you now, okay. [audience laughing] It is time. It is time for all of us to step up to prevent falls. I mean, it is really time. The good news is, there are only two steps to start the process. Are you ready? This is the first step.
Are you at risk for falls? Have you fallen in the last year? Do you feel unsteady standing or walking? Do you worry about falling? If you answer yes to any of these, you are at risk for falls. Number two. The second step is if you answer yes to any of these, I encourage you to talk to your primary care provider to one, identify your risk factors, which Laura just went over, try to minimize, and finally eliminate those risk factors for falls. Because if you don’t, this may happen. You have a fall. And I can see you in one of two places, the emergency department, or in my clinic, the Faint and Fall Clinic, or possibly both. I have had that happen too. So, if you fall, how do you know if you need to get in ASAP to be seen? Let me go through some red flags here. If you say yes, you should be evaluated right away. If you are unable to recall the fall.
I have patients that come in and they say “I don’t know, “I just found myself on the ground. “I have no recollection between when I started walking, “and I found myself on the ground. ” We don’t like that. [audience laughing] Are you hurt? Don’t minimize hurt; we need to see you. Did you hit your head? Or do you think you hit your head? Or you’re not sure? Have you been ill? Are you on a blood thinner? Dr. O’Rourke mentioned this before. Blood thinners, there’s anticoagulants; Warfarin or Coumadin, and then there are the newer anticoagulants; Pradaxa, some of you may be on those. Or there are antiplatelet medications like Plavix. Those are blood thinners. We worry when people are on blood thinners and they fall.
Next, did you lose consciousness? Some people lose consciousness and they fall, some people fall, they stand up, and they lose consciousness, we need to see you. And finally, have you had several falls? And this is number five, in just a short span, we need to see you. What’s going to happen when you come in to either the emergency department or even my clinic? We’re going to examine you very thoroughly, I call it the crime scene investigation. [audience chuckling] So, we will do blood pressure. Many times I can figure out a little bit more about you, if I do a blood pressure lying down, sitting up, and then standing up. I need to know if your blood pressure just plummets. I need to know what your heart rate does. For some of you, this may be due to dehydration. Due to some of your medications you’re on, some of it’s just due to the medications. And some of it is due to your health issues, such as heart failure, or Parkinson’s disease.
So that’s this first step we’ll do. The second and third step, may be blood tests, especially if you come into the emergency department, you’ve had a big fall, I may do an EKG looking at heart rhythm. And finally, if you are hurt, and if I need to get imaging, I’m going to do that. We’re gonna find out if you have any broken bones, or broken ribs, or if you come in at what’s happening now, is we’re teaching people how to use ultrasound. I may not be able to see all those very fine broken ribs. But if I put an ultrasound on there, I can usually find them. You’re not only going to see that in the emergency department, we’re training a lot of primary care providers on how to use ultrasound. So you’re gonna be seeing that more in your clinic, which is pretty cool. Next, if you come in, and you are particularly on a blood thinner, but if you hit your head, and if you can answer yes to any of these: over the age of 65, you’ve been vomiting, you have amnesia to the fall. I’ve heard this before, the partner comes in and says, “Well, honey, you fell.
” Like, “No, I didn’t. ” “No, you did fall. ” Blood thinner, again, there’s that blood thinner, and finally, are you disoriented? More so than at baseline, right? [audience laughing] If you have any of these we, Dr. O’Rourke and I, we’re gonna scan your head. The reason why, is because we don’t wanna miss bleeding in or around your brain. When we age, when we physiologically mature in life, a couple things happen. And one of those, is our brain starts to get smaller, it starts to shrink. No matter how much Sudoku we do, no matter how many New York Times crossword puzzles on Saturday that we try to get through, our brain is still going to shrink in size. And if we fall, our brain can actually hit the side of our skull and cause microbleeds. And over time, you may develop the confusion, the nausea, the vomiting, it may not happen the day you fall, but it may happen weeks later.
And we will always ask somebody who comes into the emergency department with those symptoms, have you fallen in the last month? It is so important. Subdural when our brain is covered, our magical brain is covered by a thick covering called the dura. And you can have bleeding on the outside of that, or on the inside of that. One of the most common bleeds that we’ll see is a subdural hematoma that’s underneath and against the brain, kinda pushes the brain aside. The other one is called an epidural hematoma. And that’s on the outside. Either way, these need to be taken care of, some of ’em can take care of themselves, if they’re very small, but others, sometimes the blood has to come out and we have to help with that. When you come in either to the emergency department or into the clinic, again, crime scene investigation, we will be asking lots of questions. And not only should we ask these questions, but if you have fallen at home or a friend, you ask these questions. Well, where did you fall? Is there a pattern here? How did you fall? Are you always falling to the front? Or do you get up and you fall backwards a lot? We need to know what time of day? Are you always falling at 2 a.
m. when you get up to go to the bathroom? I need to know that. What were you doing when you fell? Were you trying to multitask? Was the phone ringing, the dog barking, and someone asking for some water? That’s multitasking. I will give you a prescription not to multitask, as we get older. We just, we shouldn’t be doing that. I don’t like to do that. Were you carrying anything? How many of you have fallen and you’ve been carrying something, and it’s still in your arms when you wake up? Right? What were you wearing? We talked about that with shoes, and particularly shoes. Do not wear the Crocs. I don’t have stock in it, but please don’t wear Crocs. We see that a lot.
Were you using your assistive device? Do you have one and were you using it? Did you have any recent illnesses, any injuries, were there any witnesses to your fall? New or recent changes in medications, and not just prescription medications. But those wonderful medications that we see at the store that we look at the box. And we like “Ooh, I wanna look just like that person, right? “I wanna get rid of all this sinus congestion “and swing through the fields and feel great. “I’m gonna buy that. ” Well, if you combine that with some of your other medications, you could be in trouble. So what happens is, we’ll see this prescription or the prescription cascade. This happens to almost all of us. And over time, we’ll have pages of medications. Let me give you an example. High blood pressure.
Well with high blood pressure, you’re gonna be given a blood pressure pill. And a lot of these blood pressure pills, what they do is relax our vessels. And when our vessels are relaxed, I mean our veins and our arteries, blood seems to pool, so we’ll have swelling in our feet. We don’t like that. So, you have swelling on your feet, you’ll get the water pill, right? Then you’re up at night urinating and everything else. Sometimes that water pill causes dizziness and lightheadedness. That’s what caused your fall. It was all due to the prescription cascade. Well, if you combine these prescription, what happens is with the prescription cascade, eventually you’re going to be on a lot of medications. And all of these that I have listed up here, they can, especially combined together, bring you at risk for increased falls.
For example, sleep medication, we all want to sleep. I had a friend stop by, I was walking my dog yesterday and she stopped by and she said, “What do you do “for people in menopause that just wake up at night?” Well, I’ll tell you later, meet me afterwards, I’ll tell you what I told her. [audience laughing] Sleep medication, seizure medication, antipsychotic, pain medication, blood pressure, cardiac medications, antidepressants, anxiolytics, medication for anxiety, or even muscle relaxants. Many of us in this room are on one or more of these. And you combine these together, increased fall risk. The next one is what I call the fall trifecta. And sadly, we see it a little too much in Wisconsin. You have poor balance, you drink alcohol, and you’re on multiple medications. These are risk factors that you need to recognize and minimize. That is the trifecta.
The next and last two risk factors that I really wanna hone in on. I have seen so many people coming in to the emergency department, falling while texting or reading their email, while going up and down stairs. Don’t do it. I can say job security, but I really don’t want to. Don’t do that. Now the other thing that I’ve noticed lately are more people tripping on steps that don’t have any contrast or color to them. So if you think about, if you have steps going in and out of your garage or up your steps to the house, and it’s all cement the same color, certain times a day, you may not be able to see that, or if you have macular degeneration, cataracts, or glaucoma, you’re making things worse, or, and you combine that with bifocals or progressive lens and trying to find that, what they call the sweet spot to get up on that step, you’re gonna be in trouble. I highly recommend, highly encourage you to put a contrast in color on your steps. My father had terrible glaucoma, vision was so impaired we finally put, it was a physical therapist that said “Why don’t you put these yellow strips on the step?” ’cause he’d always trip on the step. No more tripping on the step, he could see the step every time he went up.
Something to think about. Finally, you’re gonna get into what we call the fear of falling cycle. If you fall, you will have a fall, you’ll fear of falling again, less activity, decreased muscle strength and balance, and an increased risk of falling. Well, guess what? We are here to help. Break that cycle, we are here to help. The UW Center for Wellness is at the American Center. They have group medical visits, they are absolutely wonderful. There is one group medical visit that I particularly would like to talk about tonight called the Wellness in Seniors Empowerment. It is a four to six week program, once a week for a couple hours I believe. Looking at successful aging, healthy aging, and falls is one of the topics that they cover.
Luckily tonight, we have Dr. Melissa Stiles who designed this program, and Katie Schwartz, the wellness coach for the program with us tonight. Dr. Stiles is in the back, can you raise your hand? There we go, Katie? [audience applauding] Thank you, thank you. They will be here afterwards to answer any questions that you may have about the program. Theirs is just one of the group medical visits offered out at the American Center, they’re absolutely wonderful. Other opportunities for us to get you healthier, are at Research Park and the American Center. These are just a minimum of the classes that we have. And I’ve chosen just these for now. But there are plenty of classes you can look at.
Living Falls Free, Aqua Yoga, Dance for Health, Mindful movements for arthritis, and Strength and Flexibility. Great classes. Finally, we have two clinics at UW for falls and we have one in the geriatric division called the UW Falls and Mobility Clinic, seeing those people over the age of 65. And for the clinic that I’m co-director of is UW Faint and Fall Clinic and we see people over the age of 18. So those are the two clinics that we have here at UW hospital, you can talk to your provider about those, getting a consult or you can self-refer as well. So I’m going to end this with, take the two steps. It could change your life. Thank you very much. [audience applauding]
– And I can see why you got the Lecturer of the Year award. That was fantastic.
It was so great that I’m not sure even where to focus, although I want a prescription to not multitask. So can I get that for you afterwards? But I would say that one of the things, that first slide pertains to almost all of us, I mean, have we fallen in the past? Are we unsteady on our feet? And do we have fear of falling? I mean I think that really hits home of looking at our risk for falls, so, thank you. Our last speaker tonight is Dr. Jane Mahoney. Dr. Jane Mahoney is a professor in the Department of Medicine, specifically in the Division of Geriatrics. She received her MD degree from UCSF. She did her residency here at University of Wisconsin, and then did her geriatric fellowship at the William Middleton Hospital VA. She is a Principal Investigator of the Community Academic Aging Research Network. She is a fantastic researcher, incredibly well-funded, she’s nationally recognized for her pioneering research for falling after hospitalization, and novel interventions to reduce the risk of falls in those of us who live in the community.
So what she’s really done is she’s conducted dissemination and implementation research, based on what we know about falling, and figured out programs for healthy aging people in the community to reduce our risk of falls. One of those is the Stepping On Falls Prevention Program, which has been widely spread across the United States. Her work is really very impressive. And Dr. Mahoney, would you please come up and finish our discussion, our talks and then we’ll discuss. [audience applauding]
– Thank you. I get the fun part, which is talking about preventing falls. We’ve heard all the doom and gloom about how bad falls are and I agree. But this is the fun part where I can talk about, yes, we can do things, these are things that we can do. So, many studies now have shown that we can reduce the risk of falling.
The U. S. Preventive Services Task Force, the American Geriatrics Society, the Centers for Disease Control, all recommend screening for falls risk and taking preventive steps. And the first step is to tell your provider if you’ve fallen. I think you’re gonna hear some things that you’ve heard before. So, it’s good that we all agree, and we all agree that telling your provider is the first step. So, once you’ve done that, and once your provider has helped you with recommendations to reduce falls, there are also things that you can do in the community setting. There are a number of evidence-based community programs, and the first one I’m gonna talk about is Stepping On. This is a seven week small group program that teaches people about strategies to reduce falls, it includes balance and strength exercises, so people can actually improve their balance and reduce their risk. And they’re invited experts, a physical therapist, a low vision expert, and a pharmacist to come to the sessions.
You can see here, this is one of the first Stepping On workshops in Wisconsin. And you can see two people doing their balance exercises very happily. And in the bottom photo, there is a physical therapist in session six, who is working with the participants on safe negotiation of curbs. Was originally studied in Australia, and where it showed a 30% reduction in falls. We, at UW working with community partners, had the good fortune to research it and package it for the United States. And our research has shown very similar reduction in falls in multiple studies. So, it works, it’s fun, people love it. And it has snacks, which we know is a key factor. [audience laughing] So Stepping On is now in 22 states and in most counties in Wisconsin, and research continues. Going on right in Wisconsin, we have done cultural and linguistic adaptations for Hispanic seniors.
And we’ve also worked with the Hmong community to adapt it for them. And lastly, exciting new work going on with people with dementia who can go together with their care partner. And we’ve done preliminary work on a Stepping Online program, which is for those who graduate from Stepping On, who then say, “I wanna do more. “I want new balance exercises to practice. ” So this is an online version that gives them new exercises, tracking a way to track that at home and progress them, and ways to have interactive features to maintain those falls strategies, that are falls prevention strategies. It’s easy to find a workshop. Safe Communities of Dane County has listings of all the workshops for Stepping On and other falls prevention workshops and programs right in Dane County, and Wisconsin Institute for Healthy Aging lists all Stepping On workshops in Wisconsin. In general, exercise programs have been shown to reduce falls. But that’s general, and the specifics are important. We’d like to be able to say that walking reduces falls, but it doesn’t.
It’s wonderful, we recommend it. But it has not been shown to reduce falls risk. What does work is balance exercises. And balance exercises reduce falls by up to 30%. That’s great news. Tai Chi, which is modified for older adults, is one of the best studied of the balance exercises, but there are others that are out there. In general, to be effective, they need to be of long duration. You’re not gonna improve your balance in one day. It’s practicing day by day over time. And they need to actually progressively challenge balance.
So that means standing exercises, it’s really hard to improve your balance when you’re sitting. So standing exercises where you’re doing weight shifts, where you’re actually making it slightly, where you have to practice your balance and practice makes perfect. One of the exciting programs which has been researched right here at UW, Tai Chi Prime is a six week program, that encourages home practice of what they call the Fab Four moves. Their idea was, if we can get some basic Tai Chi moves, and integrate them into what you do every day. So while you are making your coffee in the morning, you’re practicing your Tai Chi. If you make it easy to integrate, then you’ll practice it more, then you’ll improve your balance more quickly. That’s exactly what they showed from a six week program, significant improvement in balance, strength, and gait speed compared to a control group that was on a wait list. And most importantly, I don’t know about you. But when I took Tai Chi or another exercise program, and they said practice every day, it didn’t happen. But in this program, participants did practice a half an hour per day on average of six days per week.
So we’re very excited about this. And here’s the type of practice. This is the Tai Chi developer who’s actually practicing at the kitchen counter and with her flowers. [chuckling] And here is a senior gentleman who’s practicing what’s called the high step Tai Chi stance with his granddaughter. So, making it fun, making it easy to do at home. What else works to prevent falls? Well, I gotta start by telling you what we used to think worked, but now we know the most recent data is vitamin D does not prevent falls. The 2018 U. S. Preventive Services Task Force looked at all the research studies on vitamin D and falls, and found it no significant benefit. So, it’s no longer recommended a vitamin D supplement to reduce falls.
But, vitamin D may be helpful and still recommended by your provider for other things. First of all, if you’re vitamin D deficient, which is determined by a blood test, and second of all, if you have osteoporosis. So, if you’re trying to prevent falls, vitamin D won’t help you. But there may be other reasons to take it in discussion with your provider. Home safety. Home safety is important because half to three quarters of falls occur in the home. They occur most often in the living room, or in the bedroom where people spend quite a bit of their time. But, a fall is most likely to result in injury in the bathroom. And if you think about it, there’s very tight, narrow surfaces, narrow area to move around in, and there are a lot of very hard surfaces. So, when we focus on home safety, often we really focus on the bathroom for that reason.
An occupational therapist can evaluate your home for safety. And the result may be what you see here in the shower, with multiple handrails to make sure that that dangerous area is safe. You should also evaluate your footwear. And that you can do. We have good research that shows that walking barefoot is actually, you have worse balance barefoot, than wearing shoes. But it depends on the kind of shoes. So, shoes that improve your balance, have thin soles, very firm soles, and good heel support. And here’s a photo of that kind of shoe. That will help you with your balance. When we talk about home safety, we have to talk about pets.
[all laughing] And I’m not saying to give up a pet. They have many wonderful benefits. But, falling is not a benefit from pets. 23,000 fractures a year due to dogs and 3,000 related to cats. And I learned these statistics after a pet caused my fall. And then I realized how common it is. This is how a pet can cause a fall. This is a hallway with a dog bed in it, and you can see the dog bed with the dog in it or what looks like a dog because of the nightlight. But look at this same hallway, this is the same hallway, the dog bed is still there without a nightlight. And this is the situation I faced, when I walked into that hallway, my dog had moved his dog bed there.
Which he liked to do, and put himself in it. I fell, and the result was a fracture like this of the hip socket. [audience murmuring] And the result was six weeks of no weight bearing on the left leg, and a slow return to function. But I’m here. And now I am careful to actually do what I always tell other people to do, which is put those night lights in your house and be careful and mindful when you have pets. So in summary, to reduce your falls risk, this is really what you’ve heard this evening. Is it’s a combination of working on individual risk factors, risk related to the task, how you do your activities, and the environment. In the environment, we can reduce tripping hazards, improve lighting, install rails. We can pay more attention as we’re walking, scan ahead when we’re walking, be mindful of our movements rather than multitasking. Certainly, texting while you’re walking down the steps is not a correct way to do that task.
And we can practice safety with our pets. For the individual as we mentioned, we can improve our balance, we can improve our vision, we can minimize sedating drugs and alcohol. But all of these steps, with all of these steps together, we do know that prevention works, so thank you. [audience applauding]
– Rebecca: Well those talks were wonderful, and I’m clearly not wearing appropriate, safe shoes this evening. [laughing] So, we’ll ask all of our speakers to come up.
– Laurel: Come on up.
– And Dr. Rice and I noticed we have an all female team this evening for you. [audience applauding] Let me kick us off with the first question. What other balance exercises have been proven to reduce the risk of falls?
– Jane: So in addition to Tai Chi, there’s a set of exercises called the Otago exercises, originally done by a physical therapist.
And the exercises were actually what you saw on Stepping On. That’s a version of what we call a Otago exercises. And what we’ve realized is what they have in common, is this idea of challenging your balance and making– learning how to balance better by making things more difficult. So, you saw in that picture, people standing with one leg in front of the other. So, we have what we understand are common elements. One of the things that’s been studied most recently is some kinds of dance. And so we’re beginning to learn more, that dancing can be very helpful, not only to your balance, but to learn how to move in a way that prevents falls. So there’s a lot more to be done, but we’re starting to learn that there’s many types of exercise programs that can reduce balance, but they all have in common, this idea of you work on balance, as opposed to working on flexibility, for example.
– Here’s one, so, this is for Dr. O’Rourke.
Please define a level one trauma center, and can you tell me how rib fractures cause death?
– Ann: So a level one trauma center, the trauma centers in the state of Wisconsin are divided into four different types of trauma centers, level one through level four. And the easiest way to answer that question is what we’re prepared to do for you. Any trauma center should be able to see someone in the emergency department and stabilize them. But a level one trauma center has basically all the resources, we’re the one stop shop. And so, many patients who are seen at a level three or a level four center are transferred on to a level one center. We have surgeons in house 24/7, I’m looking pretty fresh for someone who was up all night a couple of nights ago on trauma call, I think. And so, we’re here and we have a huge blood bank, and we have operating rooms standing by, and we have neurosurgeons and orthopedic surgeons and trauma surgeons, and the CT scanners, everything we need sort of at a moment’s notice. And that is really what a level one trauma center is. Rib fractures, there’s a couple of things that rib fractures lead to patients dying from. And mostly, if you think about, if you hit your chest hard enough to break your ribs, there can also be injury to the lung underneath it, bruising to the lung, and that injured lung is at risk for pneumonia.
And even if you don’t have bruising to your lung, has anyone in this room ever had broken ribs? They’re incredibly painful. We don’t put your ribs in a cast, you have to be able to breathe, every breath you take causes those broken ribs to move, and it’s very painful. And the last thing on earth you wanna do, is take a deep breath, or to cough, and the normal things that we do, clearing our throat, bringing up little bits of secretions, it’s very uncomfortable to do. And so people don’t do that, secretions and things build up in their lungs, and patients get pneumonia. And that is really the reason for mortality in our broken rib patients.
– First, I have a comment from the audience, I took the seven week Stepping On class, it is awesome. A must do for over 65s. [cheering]
– Kathleen: Yes!
– Then some seasonal questions, as I fall in my shoes. What shoes do you recommend for summer? And any specific tips for winter walking activities?
– Jane: So for summer, I know we’d all like to wear Birkenstocks or Crocs. And actually, that’s actually not going to be the safest.
The safest is wearing these firm, thin-soled shoes with good heel support. Some people– For some people, sneakers can actually be a little bit of a falls risk. If you don’t pick up your feet, and you can actually stub your toe on ’em. For others, sneakers are fine. So it kinda varies, but I would say I agree with the, Dr. Walsh?
– Kathleen: The Crocs?
– The Crocs. For winter, there has been one study looking at what we call, you know the Yaktrax, but there’s other names for them. So I’m not recommending one item. But those, it’s like little treads that you put on your boots, and those have been shown, it was done in Marshfield to reduce outdoor falls in the winter. But the most important thing is really learning how to walk safely in the winter.
And there are safe ways to walk, partly scanning ahead, partly, really paying attention obviously. I don’t know if Laura, you have other comments on that?
– Laura: Say one more time, please.
– Jane: Going walking.
– Laura: I think you should penguin walk. [all laughing] So, if people have, for the first thing is if you don’t have to go out when it’s slippery, don’t go out when it’s slippery. But if somebody goes out to a restaurant, it starts snowing. And then they have to get to their car in the parking lot, I would have them penguin walk. So typically when we walk, we put one foot out and we land on our heel, which is a pretty small base and easy to slip on. So I would have somebody just weight shift, so your weight’s going straight down. It’s a little slower, and it doesn’t really look that ridiculous, does it? [all laughing]
– Laurel: Well, first a comment, are there any male physicians at the University of Wisconsin? [all laughing] That is cute, I like that.
Here’s another comment. I’ve got some good stuff here. Should I just wear shoes with cleats? I’m not reading that. [audience laughing] I’m not gonna go through with that, okay. So, Rebecca, you wanna go ahead?
– Sure. Great question, when will we get railings at Camp Randall? I’m not sure, any of our panel here can answer that. [audience applauding] How about this one? My balance and steadiness seem to vary day by day. Why might this be? Balance and steadiness varying. Things that can impact that, reasons.
– Kathleen: So, variability in your balance and how you feel can change day by day.
One of the things that we look at is hydration status. Dehydration can present in many, many, many different ways. And one of it is fatigue, and dizziness. And so that’s why we look at the blood pressure lying, sitting, and standing. So we encourage hydration as much as you can. And there’s your magic six cups a day or eight cups a day and that necessarily depends on who you are, if you have heart issues or anything else like that. Sometimes the medications. The other issue is how well are you sleeping that night? Have you been traveling? How much activity you’ve been doing? So there’s a lot of questions to ask on why particularly that day, you’re a little bit more fatigued and your balance is off. Usually it’s a combination of things a day or two ahead of time that caused them.
– Laurel: How much blood thinner does a one a day coated 80 milligram aspirin cause? Is that a problem? Who wants this?
– Ann: I’ll get it.
So that is a good question. And we actually argued about that here amongst ourselves. If you present to the emergency department here and you have fallen and you are taking a blood thinner, you will actually be seen by a trauma surgeon because we consider that a high enough risk for injury that we wanna do a very thorough evaluation. The one exception to that is if you take a baby aspirin. So, it definitely is a blood thinner. It affects the way your platelets, which are little tiny sticky cells in our blood that help us make clots, it effects how your platelets work, but that was where we drew the line. So the baby aspirin a day would not have you be seen by a trauma surgeon. But if you take a baby aspirin plus something else, that counts, and many of our patients take both aspirin and Plavix.
– Betsy: And I say, aspirin is not something without risk. The U.S. Preventative Task Force many of you know, the recommendation now is that no one should be on a baby aspirin a day to prevent heart attack or stroke if you have not already had a heart attack or stroke. So, that’s something you should really talk to your primary care physician about. And that’s because more mild kinds of bleeding have been shown to be more detrimental than preventing the heart attack or stroke in someone taking an aspirin.
– Rebecca: Dr. Walsh, you talked about not liking bifocals. Why?
– Oh, yes, am I on? Good. So, personally I see, probably because I see the patients I see falling, right? So not just in emergency department. But bifocals, what happened, I mean, you can have reading glasses, but if you have the regular glasses, the midrange or long-range and you have bifocals, I see more difficulty with folks trying to find that step. And it’s usually where they’re wearing the bifocals with a curb or up and down steps.
And so trying to find that spot, it’s not that you can’t wear them, but if you can switch over to a single vision lens, if you’re going out and about and you need to get up on, off and up curbs, or up and down stairs, that’s what we prefer. It’s finding that spot and I’ve seen too many people trying to multitask wearing bifocals, and they didn’t get the right spot in their glasses to see where that step was. That’s why.
– Laurel: Okay, the fall rates continue to go up. Why is that so? Who wants to answer that? Jane, you can answer this too.
– Kathleen: Well, no, well. One, we’re asking, right?
– Jane: Yes.
– Kathleen: We are asking it in Wisconsin, particularly our primary care clinic. So, our data is changing a little bit. Jane I will let you finish with that. [laughing]
– I think part of it is, we’re living longer, and we’re living longer with multiple conditions, multiple medical conditions. And we’re a very sedentary society. If we– If the combination of age-related changes, plus your medical conditions, plus being sedentary, and this can be as we’re learning, sedentary through your middle ages, you still lose ground that puts you behind when you retire and can be more active. So, we have not yet I think turned ourselves as a society into sort of the high level of prevention that we need to do. The other thing, that I think is part of this, and we were reflecting on this today, was that we are becoming more and more a multitasking society. And there’s very good data that when we multitask, our balance gets worse. And particularly if we already have balance problems. But all of us are on the go, we’ve been– this is what we do as a society. So to change our way of thinking and say, when we walk, all we’re doing is walking, that’s gonna be a big change. But I think that’s part of what we’re gonna need to do.
– Rebecca: For seniors living alone, what devices and services can you recommend to support them living independently at home and also to summon assistance if needed?
– Laura: Okay, I’ll start. So devices, so I’m not exactly sure what they mean in the question. But when I think of devices, I think of the things I showed you in the bathroom, adding grab bars, especially in places where you’re vulnerable, getting in the house, the two steps from the garage to get into the house, the bathroom, especially if you have a tub shower, trying to step over the tub. Also, if you feel like you’re losing your balance or are unsteady while you’re walking around, a cane, or a walker could do wonders for you. Make you feel more steady, you would have a higher degree of confidence in your balance, and it would lower your risk for falling. A lot of people tell me, “I don’t wanna use the walker “because I’ll look like that person. “I’m not ready to be that old yet, it has a stigma. ” And I usually ask them if that would look better than lying down on the ground face up after a fall. And I– that sounds a little brutal and harsh. But I would admire somebody who recognized and took action to prevent a fall by using an assistive device like a cane or a walker, walking sticks even.
Walking sticks are really hot right now, people take them hiking, I see them walking in my neighborhood on the sidewalk with a walking stick. Someone else had, yeah there we go.
– Betsy: Yeah, I think the other big thing is if you’re alone, Lifeline, something where you can connect immediately to an emergency service. A lot of my patients, again don’t want Lifeline ’cause the bracelet looks ugly, the necklace looks ugly, and they have their phone on them. But you never have your phone on you when you fall, I can just tell you that. I think the other thing is like Alexa, many of these devices, actually now have an option for an emergency system. If you buy Alexa, that you fall, you yell out “Alexa, “call my emergency people,” it calls your daughter, it calls your son, it calls your best friend, it doesn’t cost anything more. I think another great tip that a couple patients of mine have done who live alone is, they have a check in person and every day. They don’t have to chat, but someone just has to call and be sure they’re alive. And if they’re not, they have a system. [audience laughing] Not if they’re not alive.
– Rebecca: Not alive, yes let’s clarify that.
– If they don’t answer the phone. [all laughing]
– Jane: One more thing that I would recommend is, it’s very individualized to get the right assistive services and services in the home. And this is where seeing a physical therapist, and potentially an occupational therapist can really help you, because it depends on what’s difficult for you, how the task would be modified, or what they’ll do with the environment in terms of changes. So, I would say, as a geriatrician, my best friends are physical and occupational therapists. And so go see them. [laughing] Oh, yes, right. And with an occupational therapist, they can do home evaluations for safety. So it is a tremendous service, if you’re having problem with falls or function.
– Laurel: Are the wellness classes free or covered by Medicare?
– Rebecca: And a related question to that, while you’re answering is, do you need a referral from a health care provider to attend the strength and flexibility sessions at Research Park?
– Laurel: Oh.
– Rebecca: So do you need a referral, in addition to, are they free?
– Yes, at Research Park, you do need a referral.
– Does essential tremor result in special risk for balance and falling?
– Jane: Essential tremor, if it involves the hands is not necessarily, unless it’s causing you problems with your assistive device or holding on. There– some essential tremor can involve the head as well. And that could change your ability to sort of gauge how you’re walking safely in your environment. But there are other kinds of tremors. And those kinds of tremors are associated with problems with balance, because it comes from the same part of the brain. So Parkinson’s has a tremor and has balance problems. And then there’s– I think we’re familiar with the problems with too much alcohol can damage a part of your brain that affects balance and often causes a tremor with it.
– Laurel: So, is there any correlation between more falling and obesity?
– Ann: To my knowledge, as far as looking at the correlation and risk factors for falls, obesity has not been associated with increased risk of falls.
But, being the voice of doom, as I was asked to be, it does. Our patients who are obese do have worse outcomes from their injuries. And so, if you fall, and you have to rehab or you have fractures, they are oftentimes can be a little tougher to rehab. And some of the braces and other devices we use for spine fractures can be very challenging in patients who are obese.
– Rebecca: Any suggestions on how to land? I’m going to fall, it’s inevitable, where can I learn about landing? [audience laughing] [muffled talking]
– Jane: So, I wish that I had known how to land. But the problem is that landing happens so quickly. It’s really hard to adjust yourself, cats can. But we’re not as good at adjusting ourselves in the middle of the fall. And I did have a patient who told me, “Doc, I know how to land, and I know how to fall. ” And he never got hurt, so, but I didn’t get to ask him what his secret was.
So, we know a lot about how to get up from a fall. And that is something that a therapist can train you with Stepping On, the therapist goes over how to get up from a fall. But how to land, I don’t think we’re there yet.
– Kathleen: It is difficult, I know it was The New York Times, I remember teaching people how to fall. And it would talk about the rolling and not putting out the outstretched arms and such but then, we worry about our heads. So, I think it is difficult. But if you’ve ever been an, and like I remember I was a volleyball player, we learn how to roll when we dove on the floor. So there are techniques, you try to avoid the arms stretched out if you can, and just kinda roll but the key is dropping what you have, which is very difficult to do. We tend to have that when we are on the ground. So there’s no studies looking at the role of rolling, I guess.
– Ann: And I just wanna re-emphasize what Dr. Walsh actually said about as we age, our brains inside of our skulls are smaller, and it doesn’t matter how you land if your brain sort of sloshes around and hits the inside of your skull, you can bleed into the brain without even ever hitting your head. Just again to serve this role of doom and gloom. [all laughing]
– Rebecca: You have to finish with something better than your brain sloshing.
– I’ve been diagnosed with osteoporosis and have no cholesterol problem. What type of milk should I drink for bone health, whole, 2%, or skim? Betsy, that’s all you.
– So, it’s a Wisconsin question, no question about it. So, this is a whole, could be a whole ‘nother Mini Med is like what do we really know about diet? There’s a lot of myths about diet. Is the whole milk diet really better for you and cholesterol? And what I would say is, we don’t really know a good answer. And I would say 2% milk is the best bet right now, actually is what I would actually drink if you had osteopetrosis and need to drink milk.
And I do think in all seriousness, we are learning a lot more about nutrition. There’s a lot of urban myth out there. And it’s something we’re learning more and more about every day, and we’re gonna have some very good answers in the next few years.
– Thank you all for coming.
– Thank you. [audience applauding]
Search University Place Episodes
Related Stories from PBS Wisconsin's Blog

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport

















Follow Us