Wisconsin's EMS agencies describe a system in crisis
Staffing shortages and funding gaps in Wisconsin have caused emergency medical services to become unreliable and some EMS operations have closed, putting communities at risk throughout the state.
By Steven Potter | Here & Now
April 13, 2023
When you call 9-1-1, you expect an ambulance to show up – and show up soon.
But for some communities around the state – particularly rural ones – there’s growing concern that emergency medical services won’t be there to answer calls.
The problem? A staffing shortage.
“We have a crisis not unlike other industries like retail and otherwise,” said Alan DeYoung, executive director of the Wisconsin EMS Association. “But staffing for EMS means life and death – it means somebody’s not showing up to a call, an ambulance not arriving.”
“What we started to see in the last couple of years, departments have been closing,” he continued. “Sometimes there is a mutual aid agreement for another department to come in and help out, but many times, towns, cities, villages are without EMS. They have nobody.”
A 2023 report from the Wisconsin Office of Rural Health shows the extent of the EMS staffing problems. More than 40% of state EMS agencies had staffing gaps where no ambulance was available for emergency calls and almost 80% of EMS agencies were called to cover an emergency in a neighboring community.
“We even saw that in 10 communities, there were services that reported that an ambulance never got to a call at all – there was a 9-1-1 call requesting ambulances [but] they didn’t have staffing available and they never had an ambulance make it to a call,” said James Small of the Office of Rural Health.

James Small, an outreach manager with the Wisconsin Office of Rural Health, warns that shortages of EMS staff is leading to longer ambulance response times. “There was a 9-1-1 call requesting ambulances [but] they didn’t have staffing available and they never had an ambulance make it to a call,” he said. (Credit: PBS Wisconsin)
At the heart of the current staffing struggles is the fact that – for decades – Wisconsin’s EMS agencies have been built on and supported by volunteers.
“Right now, 79% of our state actually relies on volunteers to staff their 9-1-1 calls, which is a huge amount – a majority of the state relies on volunteers,” DeYoung explained. “Some of them might get paid a stipend, some might not get paid at all and a lot of times, they’re having to pay out of their own pocket. So we have many rural areas that are using volunteers to subsidize the cost of EMS.”

As executive director of the Wisconsin EMS Association, Alan DeYoung is sounding the alarm about a shortage of paramedics in the state. “Staffing for EMS means life and death – it means somebody’s not showing up to a call, an ambulance not arriving,” he says. (Credit: PBS Wisconsin)
To keep their ambulances staffed and on the streets, local EMS operations have had to adopt unique employment models.
“The combination model has become a popular solution,” said Paul Blount, chief for the Cambridge Area EMS agency. “So we have several individuals that work here full time. This is their full time job and then some part time members and then community volunteers-paid on-call members.”
Blount added that this varied-scale staffing set-up “helps address the need for 24-7-365 ambulance coverage.”

Cambridge Area EMS Chief Paul Blount says agencies rely on a mix of full-time, part-time and volunteer staff to provide ambulance coverage. (Credit: PBS Wisconsin)
Having started as an EMS volunteer himself years ago, Blount understands why it’s hard to keep enough volunteers to staff ambulances. “Family demands, work demands, and then it’s just a struggle to just find people to do the job and to volunteer,” he said.
A prime example of the staffing shortage is happening in Lake Mills in Jefferson County.
“Unfortunately, a bit over a year ago, we realized that we were not being successful at recruiting and retaining people,” said Jim Colegrove, vice president of Lake Mills EMS. “We were also having some financial difficulties.”
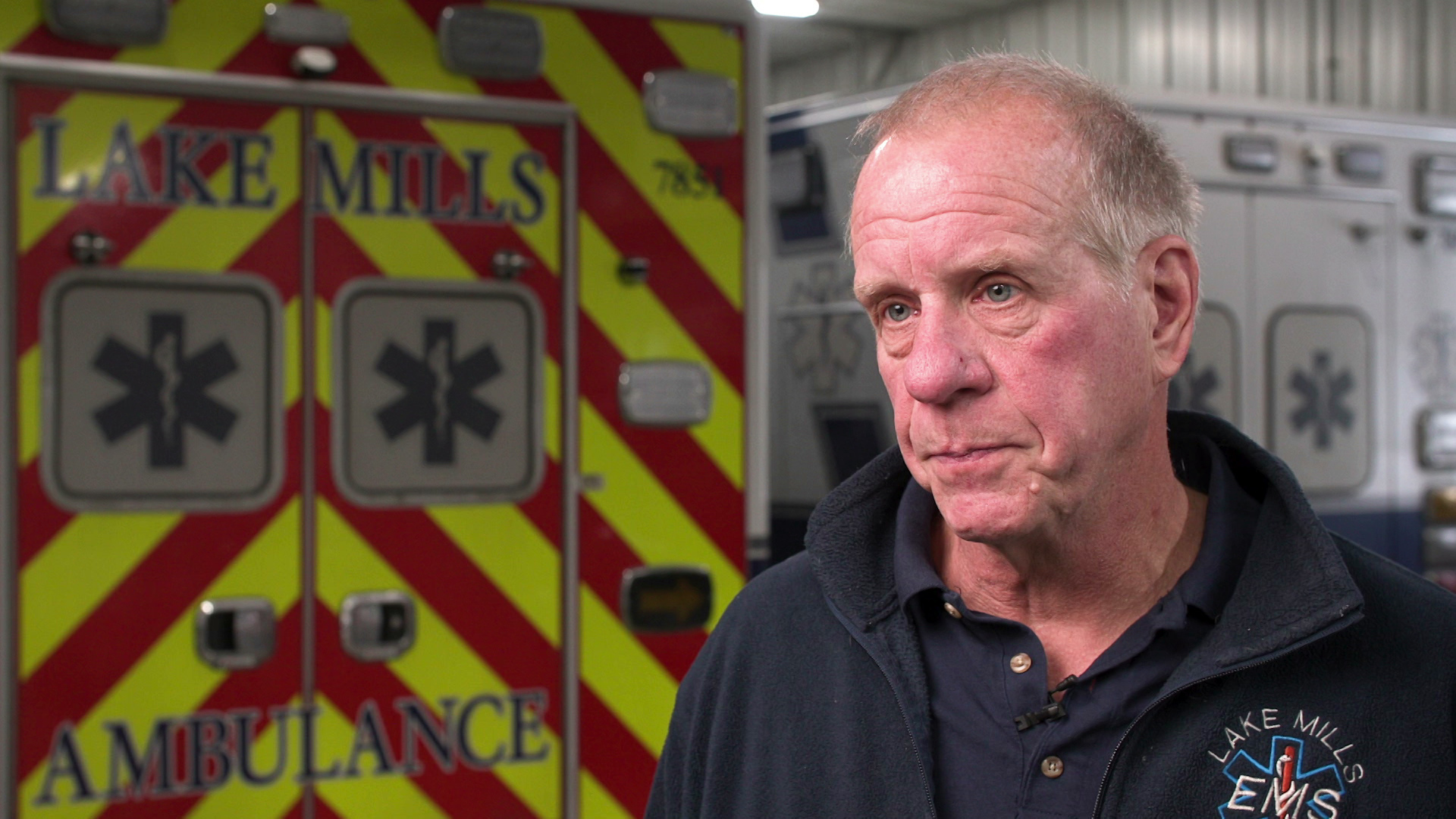
Jim Colegrove, vice-president of Lake Mills EMS, says emergency staff face intense stress on the job. “You are dealing with human beings in some of their worst possible times and you have to have a lot of empathy for those people,” he says. (Credit: PBS Wisconsin)
And now, the Lake Mills EMS operation has reached a breaking point.
“With all of that going on, we have had to make the decision that we are going to be closing our doors here on June 30,” explained Colegrove. “Because we have been serving this community, our friends, our neighbors, for close to 50 years … closing the doors is just tragic.”
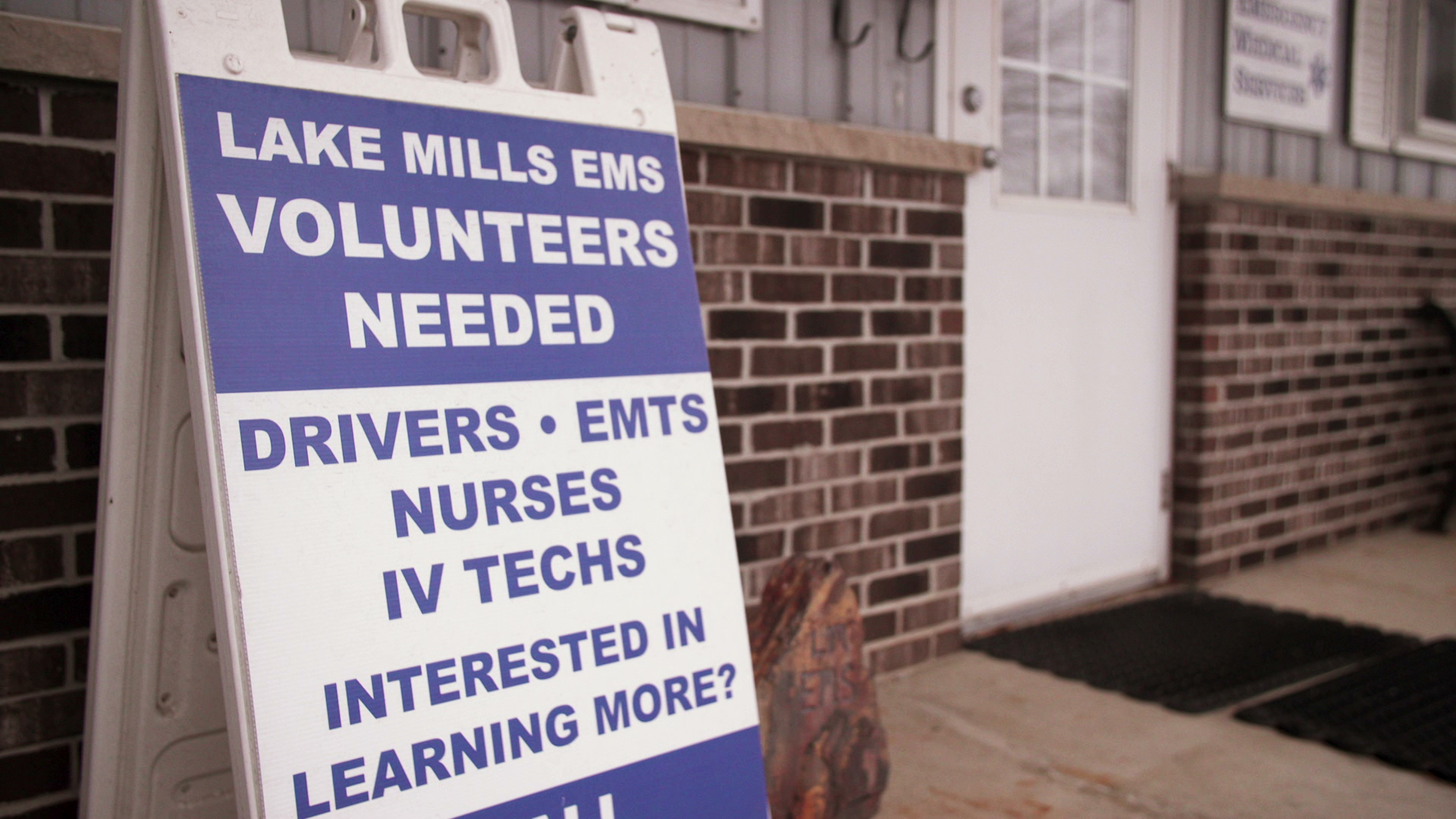
Whether you’re a paid emergency medical technician – or even an EMS volunteer – extensive training, education and certification from the state is required.
- Lake Mills EMS has been seeking more volunteers to staff its operations, but finding trained and certified recruits. (Credit: PBS Wisconsin)
- The Lake Mills EMS has had trouble recruiting new members, leading the agency to cease operations as of June 30, 2023. (Credit: PBS Wisconsin)
On top of that, Colegrove noted the work isn’t for the faint of heart.
“This is a dirty job. This is very, very difficult. You are dealing with human beings in some of their worst possible times and you have to have a lot of empathy for those people,” he said. “You have to be willing to be working in an environment where somebody is throwing up on you or doing CPR on somebody that you know who lives just down the street.”
Lake Mills is in the process of joining Cambridge Area EMS. A number of EMS agencies around the state have entered into similar consolidation agreements with neighboring communities to save money.

The Cambridge Area EMS agency will start providing service to Lake Mills in July 2023. (Credit: PBS Wisconsin)
One temporary funding solution is asking residents – through ballot referendums – for more money.
But for a long-term solution, EMS officials are seeking more stable funding from the state.
“The state really right now needs to step in, needs to provide permanent funding,” said DeYoung, adding that such funding will need to be substantial and sustainable. As a collective, he and other EMS leaders are asking for a significant amount of funding for EMS agencies around the state.
“We’re talking about $500 million in a budget, hopefully for the two-year budget here,” he continued. “That’s to provide every department about what they need – some will get less, some more based on how rural they are.”

Alan DeYoung says that $500 million would solve many problems EMS agencies are facing around the state. (Credit: PBS Wisconsin)
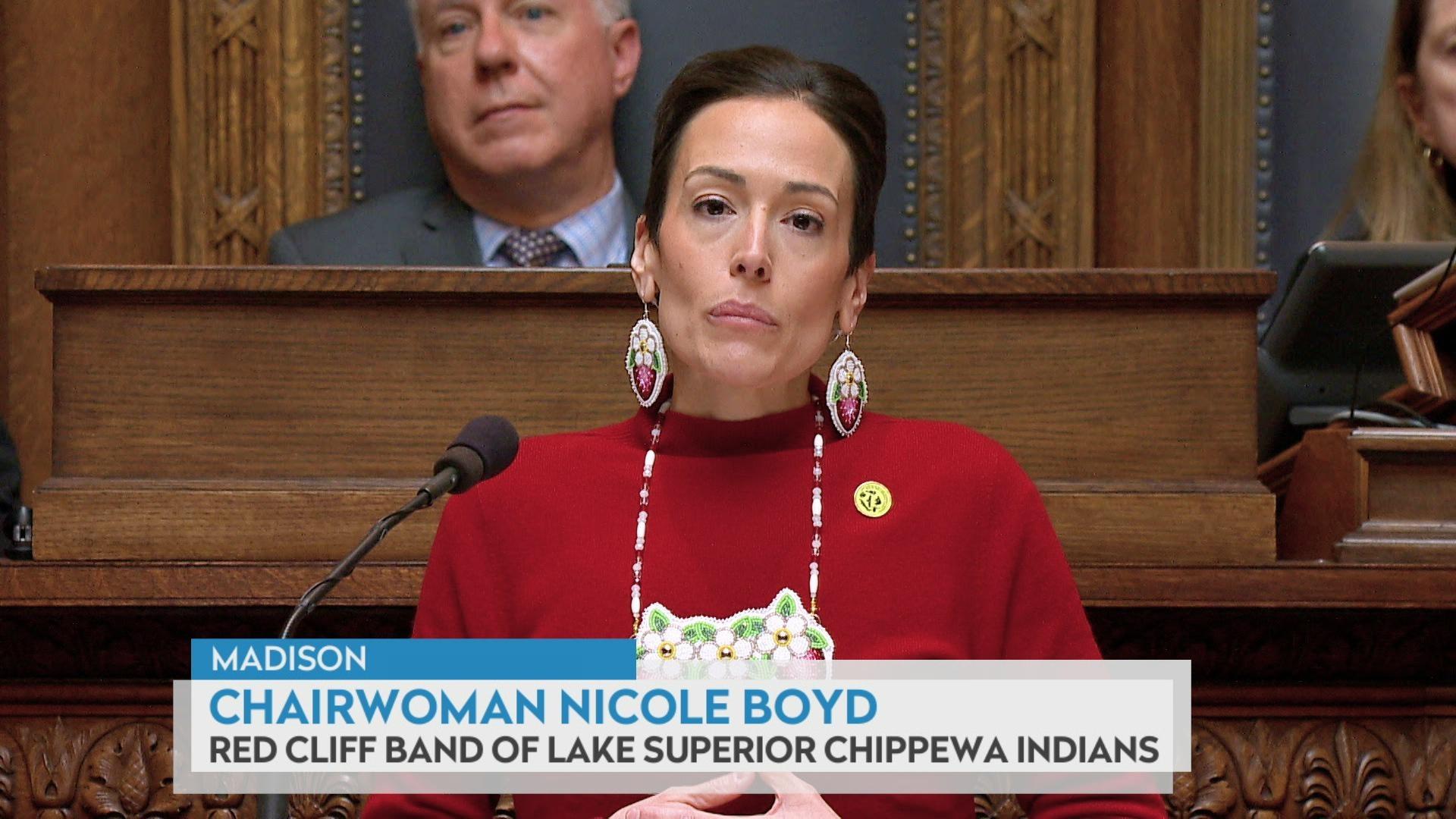
To make that funding dream a reality, EMS operators have begun knocking on lawmakers’ doors at the capitol. And, those lawmakers say they’re listening.
“As far as I’m concerned, of police, fire and EMS – EMS is the number one priority,” said state Sen. Jesse James, a Republican from Altoona.
James, who has worked hand-in-hand with EMS providers on emergency calls as a former police and fire chief in Altoona, says he knows how necessary these services are.
“It’s essential for all of us, whether you’re in the urban area or a rural area, we need to have these services available to serve our communities,” he said.
James added that he wants to explore financial incentives for smaller communities who consolidate their EMS operations.

State Sen. Jesse James, R-Altoona, a former police and fire chief, says he is interested in exploring financial incentives for consolidation of EMS agencies in smaller communities. (Credit: PBS Wisconsin)
But, he’s unsure how much Republican legislators are willing to give to EMS agencies in their state budget. “There needs to be some money put into it. I don’t know if it would reach that $500 million mark though,” James said.
EMS officials say they also need money for recruitment efforts to help them attract more potential employees to the field.
According to the state Department of Health Services, over the last decade, ambulance patient numbers have nearly doubled from about 500,000 patients per year to more than 900,000. Over that same 10 years, however, the number of EMS providers has gone from 20,000 to just 21,000 – an increase of only 5%.
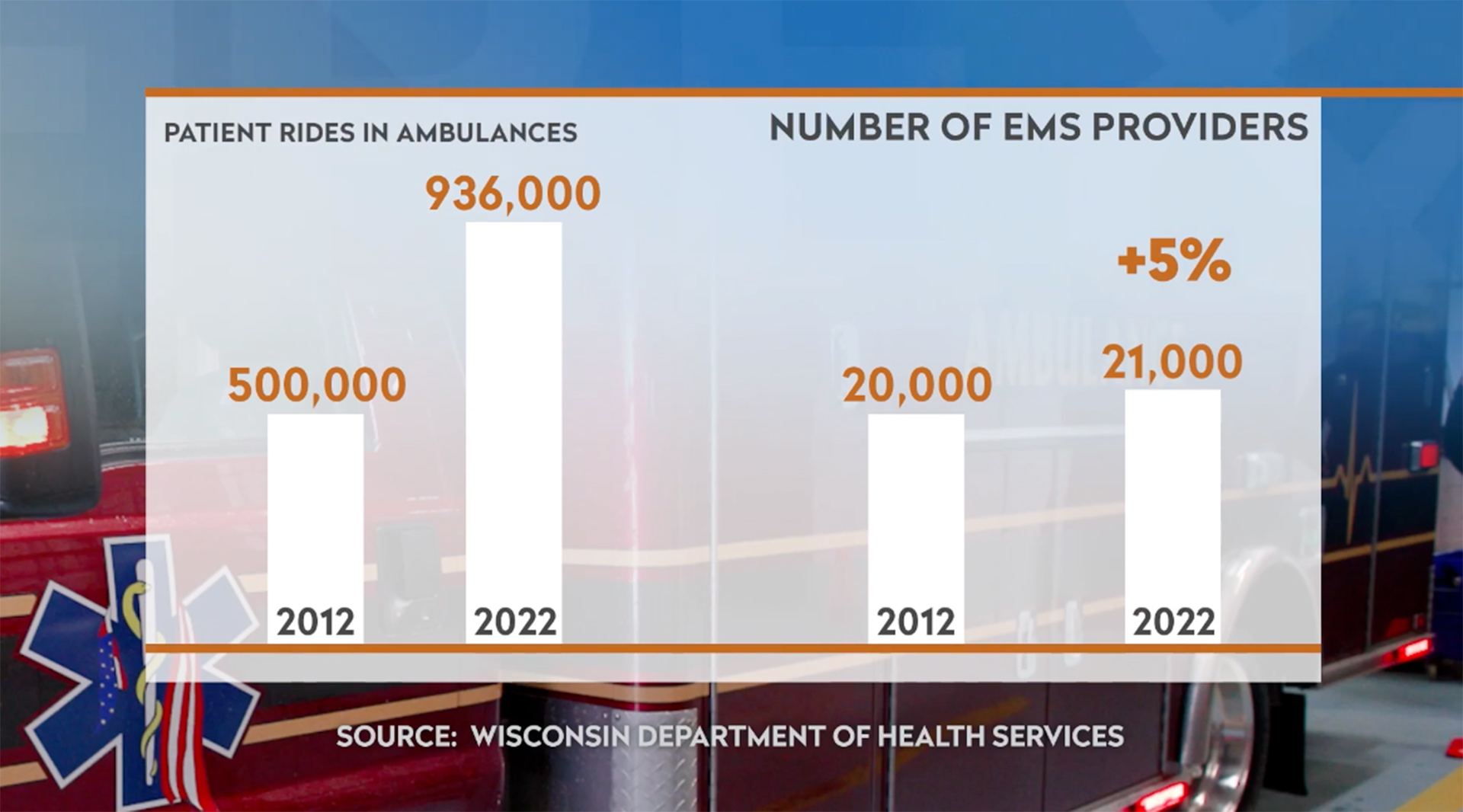
The staffing shortage in EMS responders state-wide has increased dramatically since 2012. (Credit: PBS Wisconsin)
DeYoung said those figures are about to get much worse.
“We are actually estimating about 25% of all licensed EMS providers are probably going to let their license lapse this renewal year,” he said.
Still, EMS leaders hold out hope that state lawmakers will respond to the need.
“I think that there’s definitely intent in the legislature to try to address this issue. It seems to be a very high priority. I’m getting contacted by legislators numerous times a week wanting information on the system,” said Small of the Office of Rural Health, adding that change is needed. “I don’t know what EMS 2.0 is going to look like, but we know that EMS 1.0 has run its course.”
 Passport
Passport








Follow Us