Understanding The Perennial Menace Of The Influenza Virus
Deadly global pandemics are rare enough to motivate widespread attention when they emerge, but people around the world face the threat of seasonal influenza every year.
July 3, 2020

Hemagglutinin inhibition test for influenza vaccine

Deadly global pandemics are rare enough to motivate widespread attention when they emerge, but people around the world face the threat of seasonal influenza every year. Within certain populations, the seasonal flu can rival its pandemic form in severity. Understanding the mechanism of influenza transmission assists scientists and public health officials in tracking how this virus develops and spreads.
Kathryn Schmit, an infectious disease physician in the Department of Pediatrics the University of Wisconsin School of Medicine and Public Health, discussed how the influenza virus mutates and spreads in a March 4, 2020 presentation for the Wednesday Nite @ the Lab lecture series on the UW-Madison campus. In the lecture, recorded for PBS Wisconsin’s University Place, Schmit emphasized the impact the flu can have on an annual basis.
“So far this season alone, we’re at 18,000 to 46,000 influenza deaths, which is quite a lot when we’re comparing it to some other things that are going on at this time,” Schmit said, referring to the national estimates for the 2019-20 flu season, when infections spiked. “The CDC tracks all of the leading causes of death, and in 2017, which is the most updated ones that they have, it [was] the eighth leading cause of death.”
The 2017-18 influenza season was particularly lethal, including in Wisconsin. As Schmit delivered her presentation in early March 2020, in the early stages of the COVID-19 pandemic, the 2019-20 flu season continued to be a banner concern for public health officials.
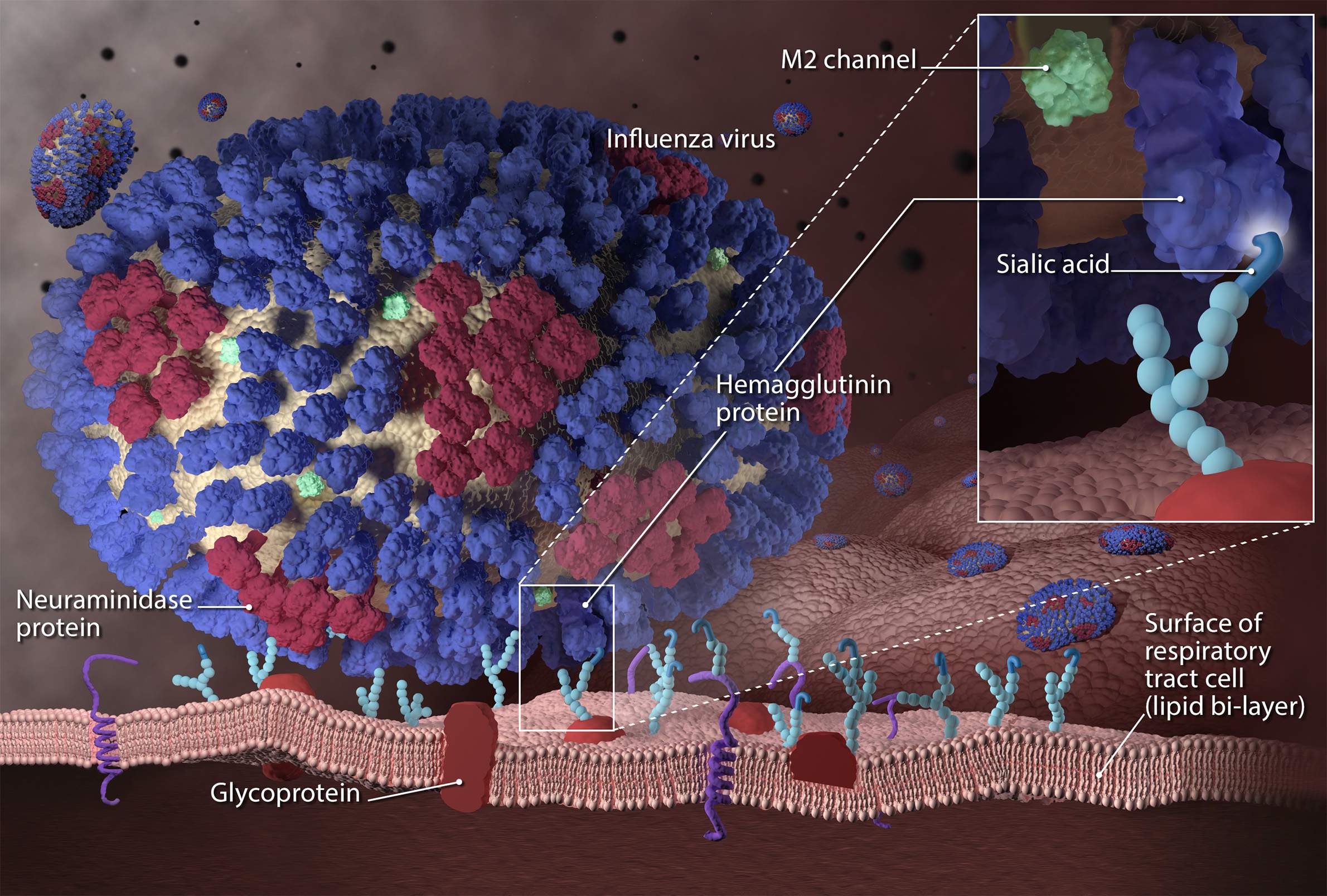
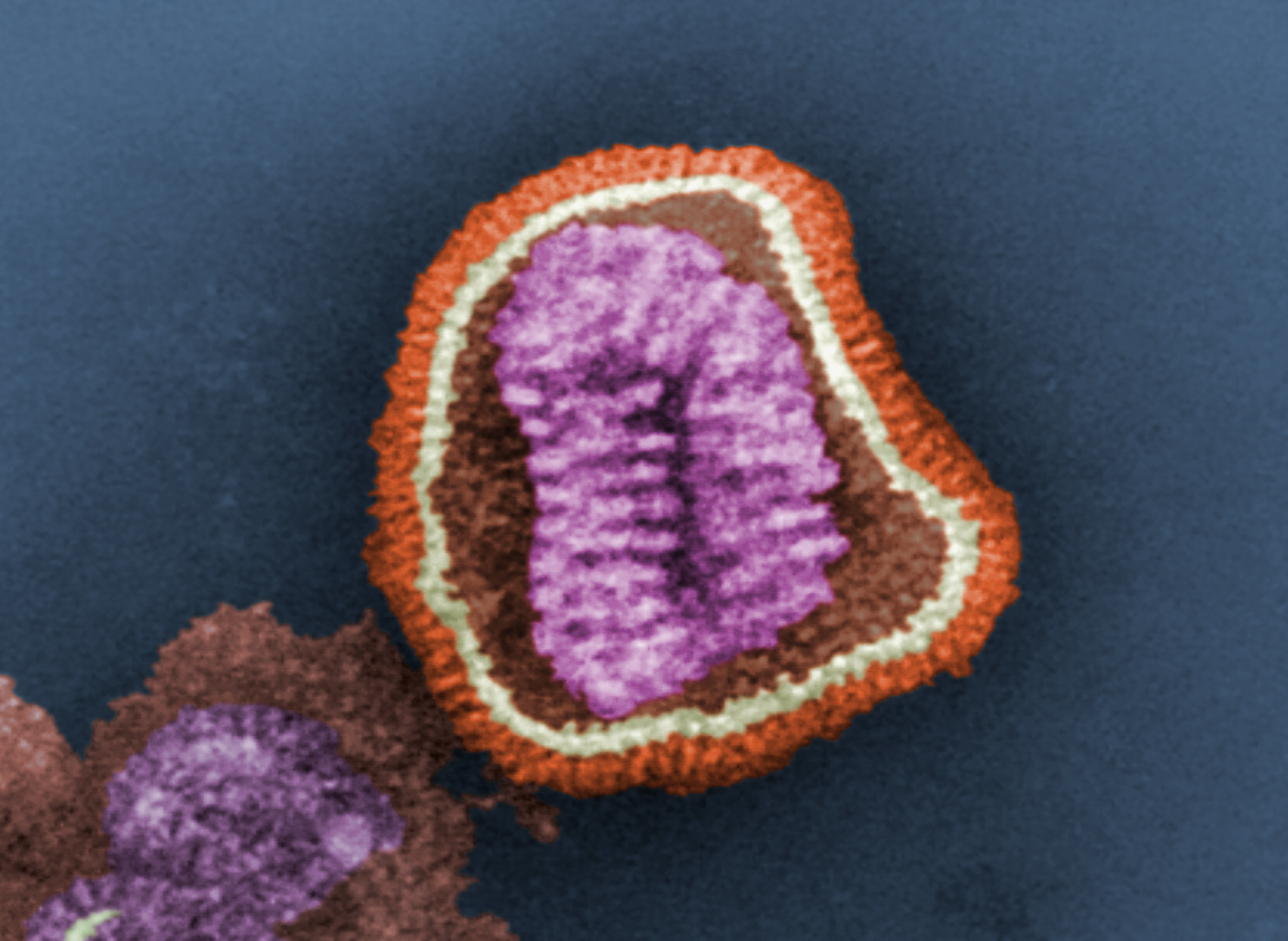
An influenza infection begins with hemagglutinin, a surface protein that helps the virus glue itself to the cells of a host animal or human. Sialic acid receptors on the surfaces of cells, which help regulate water and other biological needs, provide a ubiquitous access point for viruses.
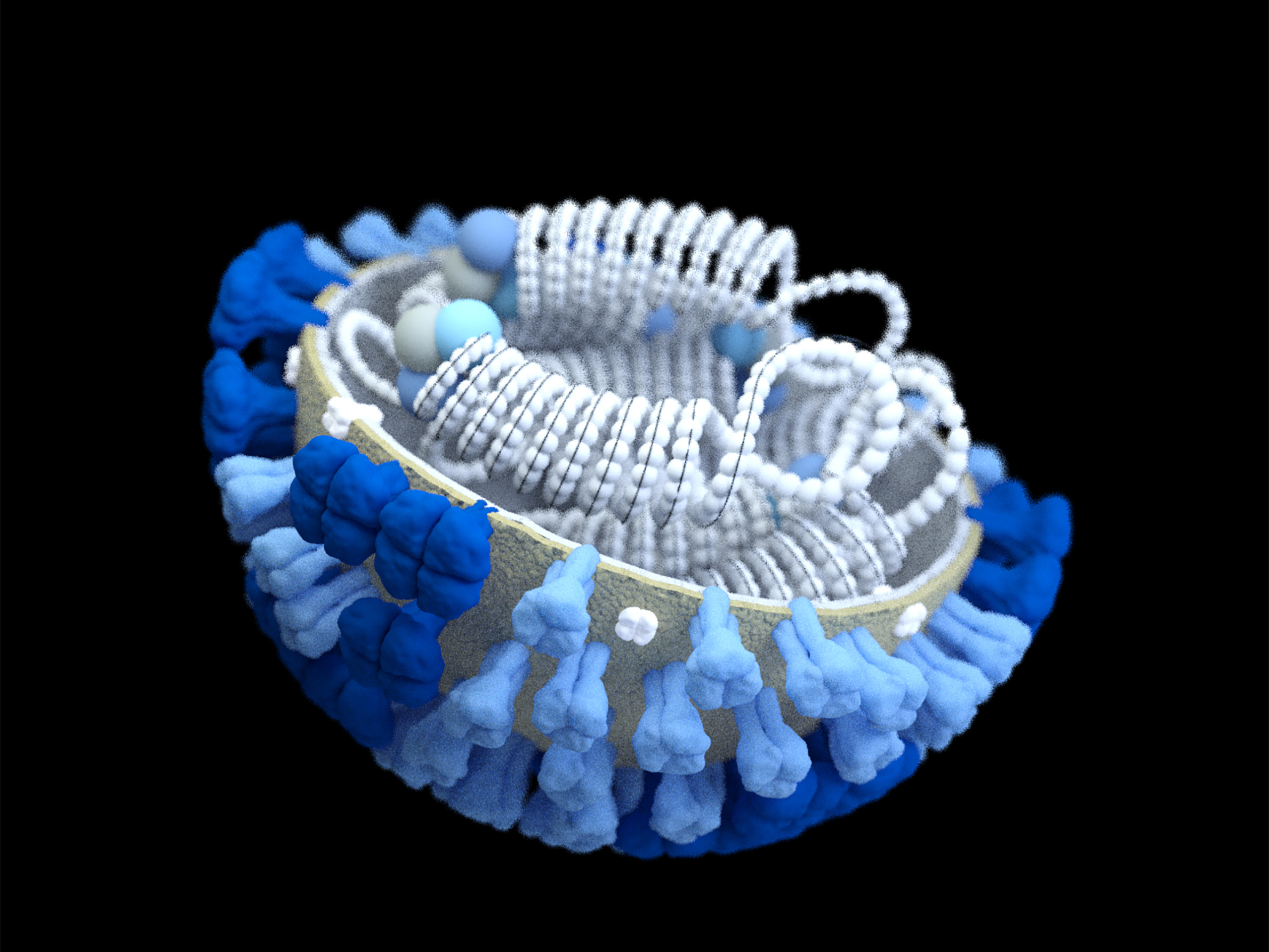
Once attached, the virus is engulfed in the cell and begins to generate new infectious particles by transferring its genetic code — in the case of influenza, ribonucleic acid, or RNA — to the nucleus of the host cell where it is replicated. When this process is complete, a second protein called neuraminidase works like a scissor to cut open the cell’s surface and release the new virus particles.
Hemagglutinin and neuraminidase are the H and N, respectively, that determine the taxonomy of some influenza strains, such as H1N1, a combination associated with influenza pandemics in 1918 and 2009. The numbers in this arrangement refer to variations in the proteins that allow the virus to mutate and fluctuate in its ability to infect and replicate.
Small changes in the surface proteins are a mechanism of change called antigenic drift.
“This is what leads to seasonal epidemics,” Schmit explained. “You have your virus, it changes slightly, but people still have some immunity to it, then that’s when you get your changes and why the vaccine may not be the best fit or why certain people are getting sick.”
A second process called antigenic shift, though similar in name, produces much more dramatic changes among influenza virus surface proteins. While organisms that have been exposed to a strain of influenza may retain some immunity when that strain undergoes antigenic drift, a novel strain of the virus created through antigenic shift will infect unexposed populations with ease, potentially resulting in deadly pandemics.
Two mechanisms drive antigenic shift: A process called spillover occurs when the virus makes the leap from carrier animals like pigs or birds into a human population. If a host has been previously exposed to strain undergoing spillover, their immune system will generally be equipped to dispatch the invading cells before the infection can spread.
The second mechanism is reassortment, and enables the influenza virus to bypass a host’s existing immunity. Reassortment occurs when a strain of influenza spills over from one species to another and combines with other strains of the virus that infect the new species. The 2009 H1N1 pandemic, for example, was the result of a spillover of genetic material from Eurasian and North American swine, combined with a previous strain that infected avian species and humans.
“So overall, there were four different species involved with it that really produced this novel or new H1N1 virus,” Schmit said. “The thing about reassortment is that it doesn’t always lead to pandemics. So reassortment can happen, we may not know that it’s happening, and as long as people are not getting sick or not dying from it, we still wouldn’t know.”
Once the influenza virus makes the leap from animal to human hosts, its circulation within and between populations is influenced by environmental circumstances and individual behaviors.
Direct contact transmission occurs when a prospective host encounters an infectious particle shed directly from an infected individual, such as when a person coughs or sneezes and releases airborne droplets.
Indirect contact transmission can occur when virus particles on surfaces end up on potential host’s hands and the person subsequently touches their eyes, nose or mouth, such as when someone with influenza coughs into their hand and then leaves traces of infected saliva on a door handle or other high-touch communal item. This method of transmission is of particular concern in the hospital environment, Schmit said.
While North America generally experiences a peak in influenza cases between September and March, this perceived seasonality is more closely tied to weather patterns than the date on the calendar. Some tropical environments see peaks in June or July, and parts of Asia may experience two peaks in a season.
“Influenza really likes colder temperatures and low humidity, so any time you alter that or change that, then influenza doesn’t do as well with circulating in the air,” Schmit said. “It would be interesting to see… what will change in the future with some of these climate changes and global warming, and what that will do for influenza, both the seasons, the duration of the seasons, and when they actually peak.”
Key facts
- While the number of influenza cases can vary widely depending on the strains circulating, as well as factors like weather and vaccine effectiveness, an average of 8.3% of the population in the United States experiences influenza symptoms each year. Influenza rates tend to be higher for children under five, and among adults age 50 to 64. The number of influenza-related deaths can vary for similar reasons, generally falling between 12,000 and 61,000 in the U.S., and 290,000 to 646,000 worldwide.
- The influenza virus has four subtypes: A, B, C and D. Type A can infect humans, pigs and birds, an ability that allows it to mutate and spread between species. Influenza A is the subtype associated with pandemics and can have the most severe impact on human health. It is also present on a seasonal basis. Type B is responsible for the other seasonal influenza outbreaks that are experienced each year, but its virulence is limited due to its ability to only infect humans. Two lineages of influenza B called Victoria and Yamagata have circulated for the past 20 years. Type C causes a mild respiratory infection in children but doesn’t lead to wide outbreaks or deaths due to its nominal symptoms. Type D is believed to only infect pigs and cattle, with no known transmission to humans.
- Pigs possess respiratory receptors for both avian and human influenzas. This trait, coupled with their large worldwide populations and often close proximity to humans in agricultural settings makes them an effective vector for influenza type A.
- During the 2017-18 flu season, the use of the influenza vaccine is estimated to have prevented 5,700 deaths and 91,000 hospitalizations in the U.S.
- The economic impact of influenza consistently numbers in the billions of dollars every year in the U.S.. The flu accounts for 45 million missed days of work and 22 million missed days of school each year, and people experiencing symptoms spend an average of $2 billion on medication to treat respiratory illnesses.
- The Wisconsin Upper Respiratory Symptom Survey is an illness-specific quality of life instrument that was used to assess the negative impact of acute upper respiratory infections in adults, developed by Dr. Bruce Barrett of the UW medical school. About 150 institutions around the world in 35 different nations use the survey to help with clinical trials and observational trials.
Key quotes
- On the early stages of an influenza infection: “The hemagglutinin, or that glue, attaches to the sialic acid receptors that are present on epithelial cells. So once it attaches to those, then the virus can then enter into your system, and then replicate, and go through the life cycle that I talked about previously. So we have these people, the susceptible individual gets the virus, the virus attaches to the sialic acid, it goes into the cell, then about one to four days after being exposed to the virus, they develop symptoms. So the one to four days is when the virus enters, and then symptoms onset, and so that’s referred to as your incubation period. So how long it takes for a person after they’ve been introduced with the virus to actually have symptoms. So relative to some other viruses, this is quite short, and so people typically present with symptoms earlier on.”
- On antigenic shift: “It’s not just a small minor point mutation change, it’s a big change. So really, you’re completely changing what the virus looks like… This occurs only with influenza A, and this is what leads to novel or new viruses that can cause pandemics. The other part of this that is important to know, that in order for these new viruses to cause pandemics, it has to be really distinct from any other previously circulating influenza viruses. So the immunity to this new virus has to be very low or none at all for it to actually cause a pandemic.”
- On the difference between antigenic drift and antigenic shift: “So antigenic drift, imagine you’re on a lazy river, right? So you’re on the tube, you’re just drifting along… and then you get stuck on the side because there’s a big bunch of people that are coming by and you get pushed out of the way. So your tube goes in a little bit, shifts a little bit, but in the end, you end up in the same spot, right? So you have a little bit of a drift, but you still end up where you wanted to be. This happens with influenza A, and it happens with B, and this is what leads to your seasonal epidemics. So if you think about it, when you got stuck in that area, you’re close to the people that you’re around in that local environment. You can transmit that virus at that point, but then you go back to your normal lazy river once the crowding goes away. Antigenic shift, you can think about it as a gear shift. So as you shift the gear, you’re ending up in a different location, or you’re going in a different direction.”
- On influenza immunization: “The important thing to know and the important thing that I like to tell patients when we’re talking about influenza vaccine is you’re 50 times less likely to get sick from influenza compared to someone who doesn’t get the vaccine. I feel like this is an important concept that we don’t talk about very much.”
- On the potential for future pandemics: “Overall, experts are really focusing on the avian influenza and their concern about the avian influenza actually causing the next pandemic. And the reason for this has to do with, there’s two current strains of avian influenza that have actually gone to humans at this point. The first one is something called H5N1. So H5N1 started to become present in 1994 when they first noticed that there was a new strain in humans when someone got very sick, and they’ve been tracking it. It’s kind of spread throughout different continents. It’s been present in Europe, it’s been present in Asia, it’s been present in North America.”
 Passport
Passport








Follow Us