How Does Wisconsin's Pre-Existing Conditions Proposal Line Up With The ACA?
In January, the Wisconsin Assembly passed a bill that addresses pre-existing conditions, but the scope of this proposal does not overlap completely with what is defined by the ACA.
By Will Cushman
February 5, 2019

Hand holding insulin pump

The state of Wisconsin’s involvement in a multi-state federal lawsuit seeking to overturn the Affordable Care Act was a central issue in the fall 2018 statehouse elections. One particularly potent aspect of the political debate was, and remains, what would happen to people with pre-existing medical conditions if the law were to be overturned.
The ACA defines a pre-existing condition as any medical problem, from obesity to asthma to diabetes to cancer, that begins prior to new health insurance coverage taking effect.
Before President Barack Obama signed the ACA into law in 2010, there was no nationwide law requiring insurers to offer health plans to customers with pre-existing conditions. Some states passed laws prior to the ACA that required insurers to cover pre-existing conditions. However, such laws often led to skyrocketing premiums and insurers leaving state insurance markets rather than sell plans to people with pre-existing conditions.
The ACA bans insurers from refusing customers with pre-existing conditions nationwide. The law originally included several provisions meant to help control costs of insuring customers with pre-existing conditions, including subsidies and a mandate that all people purchase health insurance or pay a tax. That mandate was overturned in 2018 in a tax bill passed by Congress and signed by President Donald Trump. The subsidies remain in place with the rest of the ACA, though, as the multi-state lawsuit to overturn the law works its way through the legal system.
Voters nationwide and in Wisconsin have consistently rated the provision for coverage of pre-existing conditions as one of the most popular parts of the ACA. Republican proponents of the multi-state federal lawsuit in Wisconsin, including former Gov. Scott Walker, pledged during the 2018 campaign to pass a state law requiring insurers to cover pre-existing conditions should the ACA be overturned in court.
In December 2018, a federal judge in Texas ruled the entire ACA invalid, but stayed the ruling pending an appeal by the 16 states that support the law that is forecast to go before the United States Supreme Court.
In January, the Wisconsin Assembly passed a bill that addresses pre-existing conditions, with nearly all Republicans and about half of the Democrats voting in favor. But the scope of the Wisconsin proposal does not overlap completely with what is defined by the ACA.
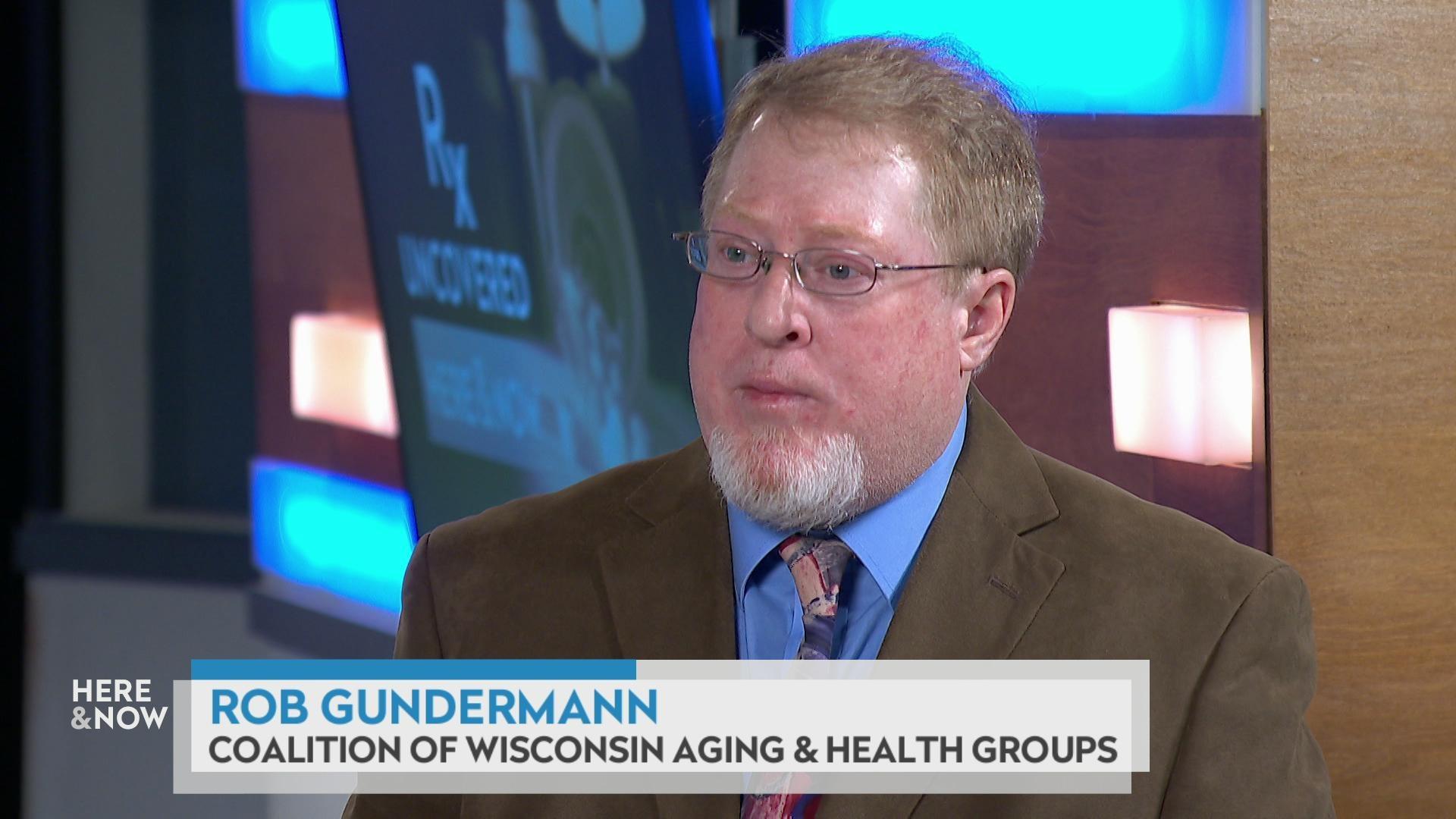
Donna Friedsam, the health policy programs director at the University of Wisconsin-Madison’s Population Health Institute, spoke on the Jan. 25, 2019, episode of Wisconsin Public Television’s Here & Now about the bill and how it compares to the regulations set out in ACA.
Friedsam said the Wisconsin proposal would “protect people to a certain degree, but not as completely as it might seem.” There are two major differences between the state legislation and current federal law, she explained.
First, the ACA requires insurers to offer health plans that cover a set of essential health benefits. While the Wisconsin bill would require insurers to sell coverage to patients with pre-existing conditions, Friedsam said it does not specify what benefits health plans must cover.
“Even if plans are required to cover people with pre-existing conditions, [insurers] might sidestep this by offering plans that do not cover the services or prescriptions needed for certain conditions,” Friedsam said in a follow-up interview with WisContext.
Second, as a federal law, the ACA is able to regulate all forms of health insurance, whereas any law passed in Wisconsin would only have the ability to regulate some forms of health insurance. State law cannot regulate “self-insured” health plans, Friedsam said, which are employer-provided health plans regulated by a 1974 federal law called the Employee Retirement Income Security Act (also called ERISA).
About 61 percent of Wisconsin’s employers offer self-insured plans, Friedsam said, and about 1.5 million Wisconsin employees work at firms offering such coverage.
“The state law [would] not have any effect on how these self-insured plans operate,” Friedsam said, though she noted that most self-insured plans are offered by large employers that are likely to continue offering coverage for pre-existing conditions without restriction because they’ll have the means to do so.
That’s not likely to be the case for employees at smaller firms, she said.
“About 80,000 Wisconsin employees work for small firms that self-insure, and these firms may consider cutting back on the scope of their insurance coverage,” Friedsam said.
The bill has yet to be taken up by the state Senate. Many Democrats, including Gov. Tony Evers, have criticized the bill’s provisions as inadequate, saying it would make health insurance effectively out of reach for many people with pre-existing medical conditions. Assembly Republicans and Evers did negotiate a deal for the proposal to ban yearly and lifetime coverage caps for people with pre-existing conditions, a provision that was not in the original language of the bill.
 Passport
Passport









Follow Us