Wisconsin's Covid Condition: Omicron looms as Delta continues crushing hospitals
A year after the state's worst surge of the pandemic to-date started subsiding, the Delta variant of the coronavirus keeps fueling rapid growth in new cases and hospitalizations, even as the potentially highly transmissible Omicron variant threatens to emerge.
By Will Cushman
December 3, 2021

A highway sign in front of the William S. Middleton Memorial Veterans Hospital in Madison on Dec. 3, 2021 is a sign of the ongoing pandemic. (Credit: Will Cushman / PBS Wisconsin)
The world’s attention turns to yet another coronavirus variant, even as Wisconsin’s hospitals are increasingly overwhelmed with COVID-19 patients stricken by an earlier variant. More than three months after the latest wave of the pandemic hit the state, average daily case counts, hospitalizations and deaths are continuing to grow, with the number of covid patients needing a ventilator reaching an all-time high in Wisconsin.
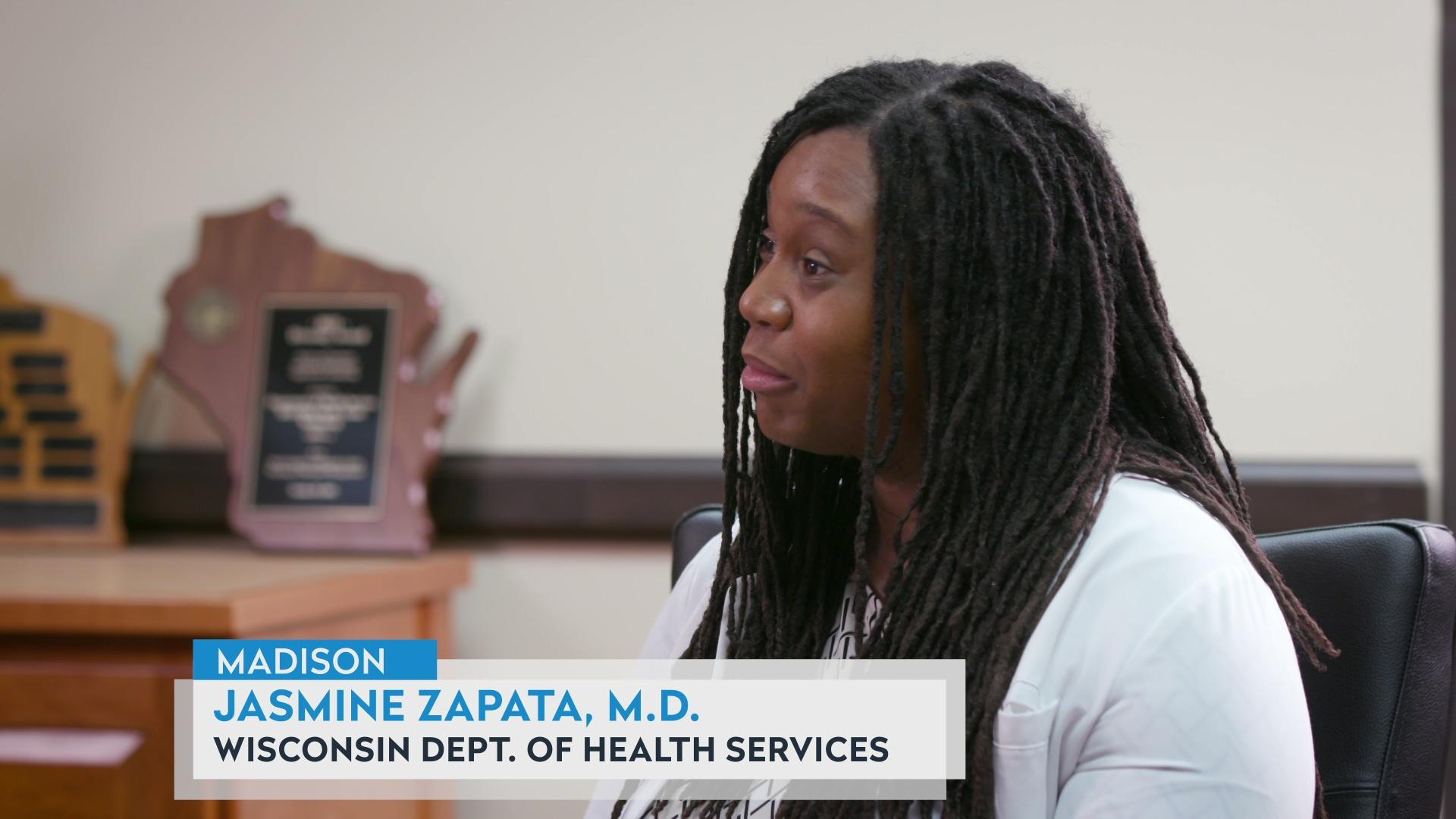
Wisconsin Department of Health Services data show unvaccinated people are at much higher risk of being hospitalized and dying from COVID-19, and public health officials are imploring Wisconsinites to get vaccinated and to get a booster shot. As the Delta variant onslaught persists and early evidence suggests the Omicron variant is poised to present an additional challenge to Wisconsin’s beleaguered hospitals, officials continue recommending precautions like distancing and mask-wearing over the winter holidays. Here’s the status of the COVID-19 pandemic in Wisconsin.
Delta surge deepens
Wisconsin’s long-building COVID-19 surge fueled by the highly transmissible Delta variant of the SARS-CoV-2 virus is showing no signs of abating months after it was first identified in the state in August 2021.
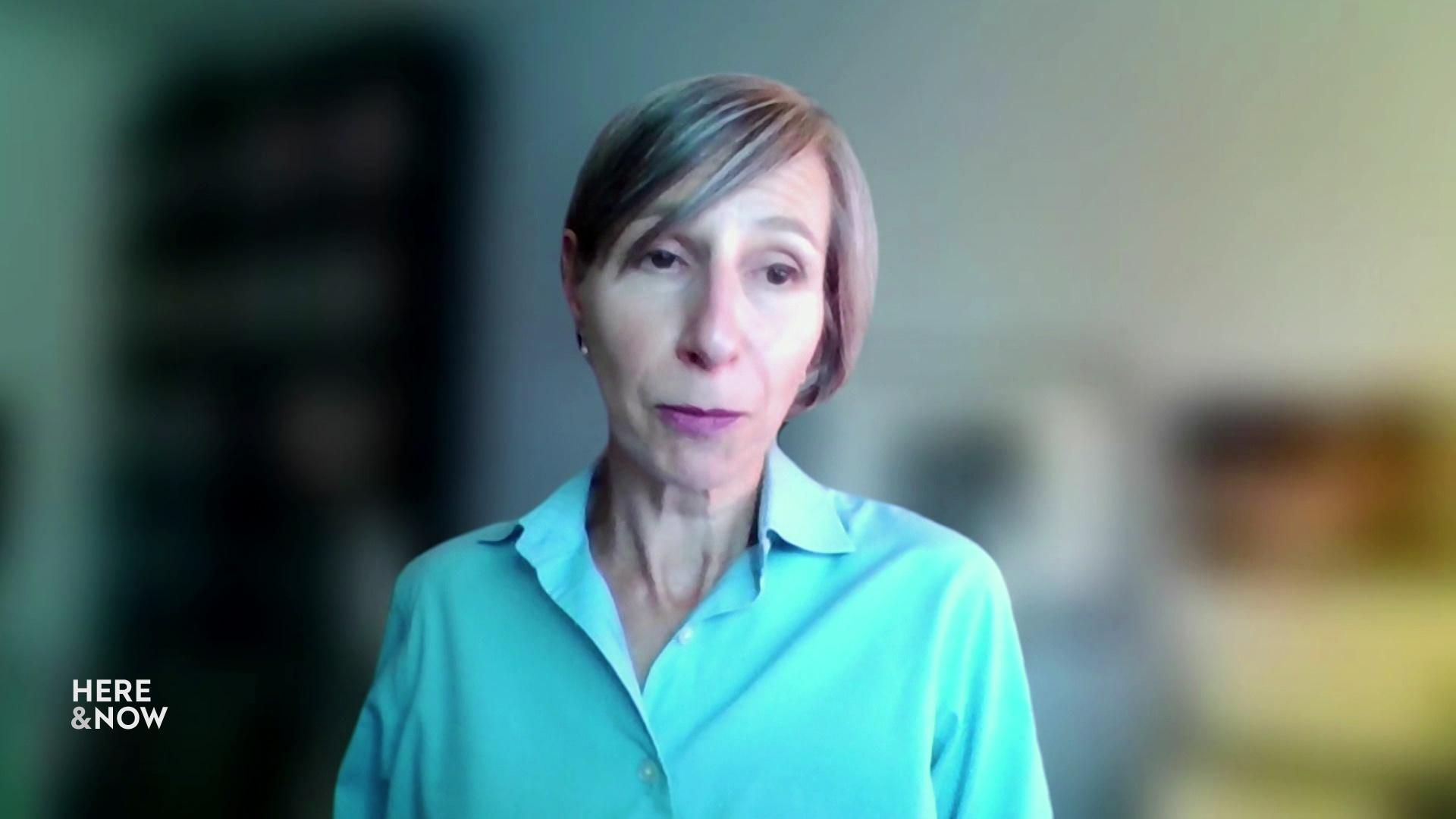
Karen Timberlake, Secretary-designee of the Department of Health Services, noted during a Dec. 2 media briefing that while the Omicron variant is raising serious new concerns about the trajectory of the pandemic, the health-care crisis in Wisconsin remains dominated by Delta.
“As of today, Delta remains the dominant variant in Wisconsin, as in the U.S., and is found in more than 99% of the virus samples that our lab partners evaluate,” Timberlake said.
After a brief reporting dip related to the Thanksgiving holiday, when testing slowed, the state’s 7-day average for new confirmed cases topped 3,000 once again on Dec. 1, the same day the agency reported nearly 5,100 new confirmed cases, a daily high for 2021. Just one day later, the average climbed to 3,548, its highest level since mid-December 2020.
Confirmed cases represent only a portion of all new infections, as this designation requires laboratory confirmation of the coronavirus’s genetic material within a sample taken from somebody who gets tested. This type of testing is not as widely accessible as during the first year of the pandemic. It’s also time-consuming, and people seeking convenience and faster results are increasingly turning to at-home rapid tests that detect the likely presence of the virus in a different, less precise way.
The state health department counts positive results reported from these rapid antigen tests as probable cases. On Dec. 2, the 7-day average for new probable cases rose to 673. That’s easily its highest level throughout the pandemic to-date, including during the worst surge of confirmed cases yet seen in Wisconsin, which peaked in November 2020.
As case counts indicate, the virus is once again out of control around the state, with 26 counties experiencing “critically high” transmission and the remaining 46 counties experiencing “very high” transmission over the 2-week period ending Nov. 30, according to state data.
The long surge is leading to a sustained rise in covid-related deaths in Wisconsin. On Dec. 2, the 7-day average for newly reported deaths rose to 24. An average of about a dozen or more state residents have died from COVID-19 every day since early September.
According to the state health department, in October unvaccinated and partially vaccinated Wisconsinites died from covid-related causes at a rate 15 times higher than those who were fully vaccinated.
While Delta remains dominant in Wisconsin, early evidence from South Africa, where the Omicron variant was first detected in late November, shows it is likely even more transmissible than Delta and better able to evade immunity derived from prior infection and vaccination. That’s according to Dr. Michael Osterholm, an epidemiologist and director of the Center for Infectious Disease Research and Policy at the University of Minnesota. Osterholm weighed in on the new variant during a Dec. 3 interview on Here & Now.
Calling the threat Omicron poses to public health “a real concern,” Osterholm pointed to growing evidence that the variant’s many mutations help it infect more people more quickly than previous strains of the virus.
“Early data shows us that many, many individuals who have been previously infected in South Africa are getting infected again,” Osterholm said. He noted that it remains too early to know how often the variant causes severe illness compared to Delta and other variants, though he added that hospitalizations in South Africa have started to rise.
President Joe Biden announced stricter rules for traveling to the United States in response to the variant. He also outlined a nationwide strategy for combating Omicron, including improving Americans’ access to rapid testing and making sure those who are eligible can easily get covid vaccine booster shots to boost their immunity.
Wisconsin health officials said during the Dec. 2 briefing that while Omicron had not yet been detected in Wisconsin, it was likely to turn up soon and may indeed already be present. Asked whether the variant would prompt changes to public health guidelines, Timberlake said it is too early to know. She recommended sticking to strategies known to be effective in driving down transmission of other variants, such as vaccinations, booster shots, indoor mask-wearing in public, and getting tested and staying home when sick.
“As far as any of us know right now, [these strategies] will all be the right things to do if and when the Omicron variant does start to circulate more widely,” Timberlake said.
Hospitals again overburdened
With the possible threat of another dangerous variant hanging over the state, daily hospitalizations related to COVID-19 rose to a new high for 2021 in early December.
On Dec. 3, the Wisconsin Hospital Association reported 1,457 covid patients were hospitalized across the state, the highest number since mid-December 2020. Many of those patients were seriously ill, with more than one-quarter of those hospitalized in intensive care units.
Nearly 700 patients across the state were on ventilators as of Dec. 3. That figure includes both covid and non-covid patients, but the 699 patients counted on that date represented a high point since the pandemic struck Wisconsin in March 2020.
Hospitals across the state were seeing more covid patients following the Thanksgiving holiday, with hospitalizations climbing particularly quickly in hospital regions encompassing northwest, north-central and south-central Wisconsin.
In Green Bay, one overburdened hospital operated by Prevea Health was recently forced to turn away 28 patients, including three who had suffered strokes, on a single day, according to Dr. Ashok Rai, its president and CEO. Rai spoke at the Dec. 2 media briefing with state health officials.
“This wouldn’t happen if we had those beds … which are now being occupied by covid patients,” Rai said. He noted that the number of staff available to treat covid patients is often a more limiting factor than physical bed space.
“COVID-19 patients are extremely labor intensive,” Rai explained, noting that a single covid patient can require up to three times as many resources as a patient for another common disease.

A lawn sign points toward a COVID-19 testing clinic located in the parking lot of the Warner Park Community Center on the north side of Madison. (Credit: Kristian Knutsen / PBS Wisconsin)
Meanwhile, seasonal flu is beginning to circulate in Wisconsin. More influenza cases were reported in a single week at the end of November than during the entire previous flu season. Covid-related public health precautions helped keep flu to a minimum over the winter of 2020-21, but fewer restrictions are in place a year later. Dane County is the only place in the state that has renewed county-wide mask mandates in response to the Delta surge, with the latest extended to Jan. 3, 2022.
Dr. Ryan Westergaard, the state’s chief epidemiologist for communicable diseases, said it’s too soon to know what impact influenza might have on Wisconsin’s health-care resources over the winter.
“We don’t know what to expect with this influenza season,” Westergaard said during the Dec. 2 media briefing. “But there are reasons both for concern and also potentially for optimism.”
Westergaard said the extremely low number of flu cases seen during the previous winter indicated that strategies aimed at preventing COVID-19 transmission also worked very well against flu, though he noted that the pace of influenza vaccinations in 2021 was slower than usual.
“We haven’t been paying enough attention collectively to encouraging influenza vaccination during the second year of the covid pandemic,” he said.
Winter is typically the busiest time for hospitals as influenza and other seasonal respiratory illnesses peak. Preventing Wisconsin’s hospitals from being crushed by an onslaught of new patients would depend on taking precautions against both covid and the flu, Westergaard said.
 Passport
Passport









Follow Us