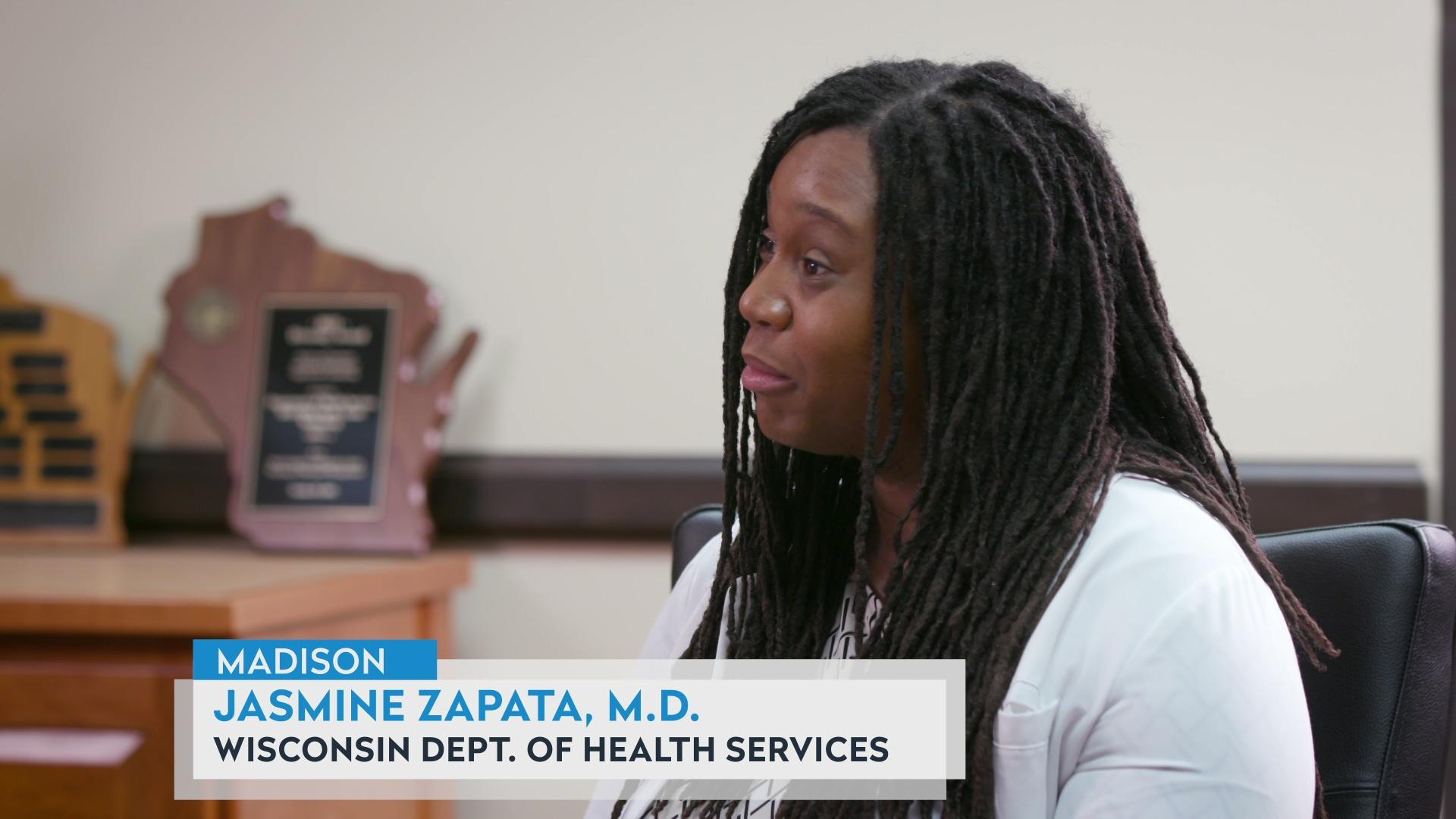
Northeastern Wisconsin Grapples with Hospitalizations
By Frederica Freyberg | Here & Now
October 16, 2020 • Northeast Region
Emergency Department Medical Director at Bellin Hospital in Green Bay Dr. Paul Casey talks about how the region’s hospitals are handling the influx of COVID-19 patients.
 Passport
Passport









Follow Us