A Trio Of Nurses Share The 'Surreal' Ordeal Of Fighting For Lives In A COVID-19 ICU
Over several interviews, a trio of nurses offered an inside look into how frontline workers are responding to the virus that has upended life in Wisconsin.
April 13, 2020

Intubation on simulated patient at Fort McCoy illustration

At 3 a.m. on a recent weekend, “Marcie’s” phone pinged with a text from “Sarah,” a fellow nurse in a COVID-19 intensive care unit at a Madison hospital.
A house was for rent on Craigslist, Sarah texted, suggesting that they rent it to avoid getting their families sick. Marcie would do it, she texted back, but was “limping along financially.”
“I’ll pay for your portion so your boyfriend can stay safe from this,” Sarah replied.
Spurring the early-morning exchange: anxiety that now envelops nurses caring for patients succumbing to the widening novel coronavirus pandemic.
Sarah and Marcie — not their real names — are used to witnessing pain and death at work. But it was nothing like what they are confronting now.
Marcie described the atmosphere in her hospital as “surreal,” as once-healthy patients struggle for breath and suddenly die, while the nurses who care for them fear going home and bringing the disease back to their loved ones.
Over several interviews, Sarah, Marcie and a third nurse, “Justine,” offered an inside look into how frontline workers are responding to the virus that has upended life in Wisconsin.
The Cap Times and Wisconsin Watch granted anonymity to the nurses, who feared reprisals from their managers. Stories abound of U.S. hospitals firing staff who publicly describe conditions during the pandemic. The news organizations are leaving the hospital unnamed to further protect the nurses’ identities.
Sarah is “not typically a crier” but now occasionally bawls while biking home from work. Marcie, a self-described “crusty old ICU nurse” — an even-keeled and sober presence in her critical care unit — said she now cries every day. She fears for her patients. She fears for her family. She fears the unknown.
The nurses said the virus has left them “shell shocked,” and without enough personal protective equipment, or PPE, to stay safe from an expected onslaught of patients. Supplies are in “crisis” mode — workers repeatedly reuse masks and rub hand sanitizer on their gloves instead of throwing them away – even before the full crisis has hit the hospital, Justine said.
As of April 13, 2020, 3,428 Wisconsinites had tested positive for COVID-19 — 993 of whom were hospitalized, while 155 people have died. Limitations on testing mean the true numbers are likely higher.
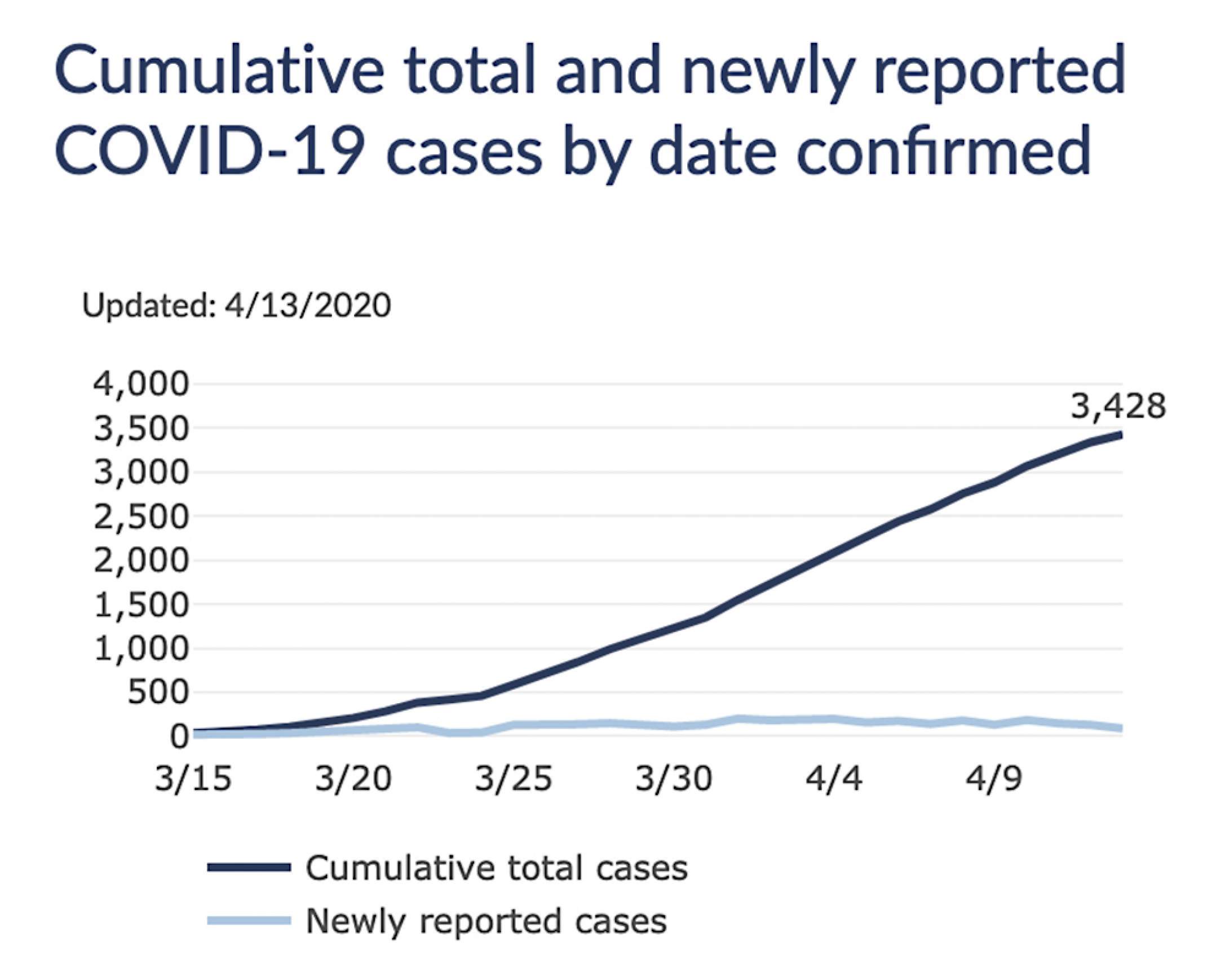
In Milwaukee County, 1,743 people have tested positive. In Dane County, Wisconsin’s second-largest county, the number stands at 340.
Wisconsin Department of Health Services models predict novel coronavirus cases will peak between April 23 and May 23.
University of Washington researchers at the Institute for Health Metrics and Evaluation project Wisconsin to reach peak hospital resource demands on April 14. The state will still have enough ICU beds, the researchers predict, although that projection, which is updated three times a week, can change depending on how well the public practices safe physical distancing.
Nurse feels like a ‘pawn’
Dr. Ryan Westergaard, chief medical officer of the Wisconsin Department of Health Services’ Bureau of Communicable Diseases, has said there is evidence that Wisconsin is succeeding in flattening the curve — or spreading the number of cases across a longer period of time. But experts fear that the long lines and wait times endured by voters in the April 7 election will cause a spike in cases in the weeks to come.
The atmosphere of the ICU has a new tenor of anxiety as nurses fight an invisible and unfamiliar enemy. There’s also anger.
Justine said she’s disappointed that manufacturers haven’t delivered more personal protection equipment, angry that an election was held during a pandemic and betrayed by politicians who praise frontline workers yet fail to deliver the supplies needed to keep them safe.
“It’s like I’m the pawn in a game of chess — and I’m a sacrificial lamb,” she said.
About one-third of Wisconsin hospitals have a supply of N95 masks that will last seven days or less, according to data from the Wisconsin Hospital Association. Roughly half of the state’s hospitals are a week away from running out of face shields, goggles and gowns, WHA says.

At daily meetings, the hospital has reminded the nurses not to talk to the media unless they are approved to do so. Doctors and nurses at other hospitals elsewhere have been fired for speaking to the media about COVID-19, something Sarah called “complete bullshit.”
“Doctors and nurses who are talking to the media are trying to make the public aware of what’s going on, companies aware of what’s going on, and to pay attention and encourage people to do social distancing and be careful,” she said.
Public health officials believe a surge of COVID-19 infections is coming, and that many of these patients will need to be hospitalized.
Most cases mild — some deadly
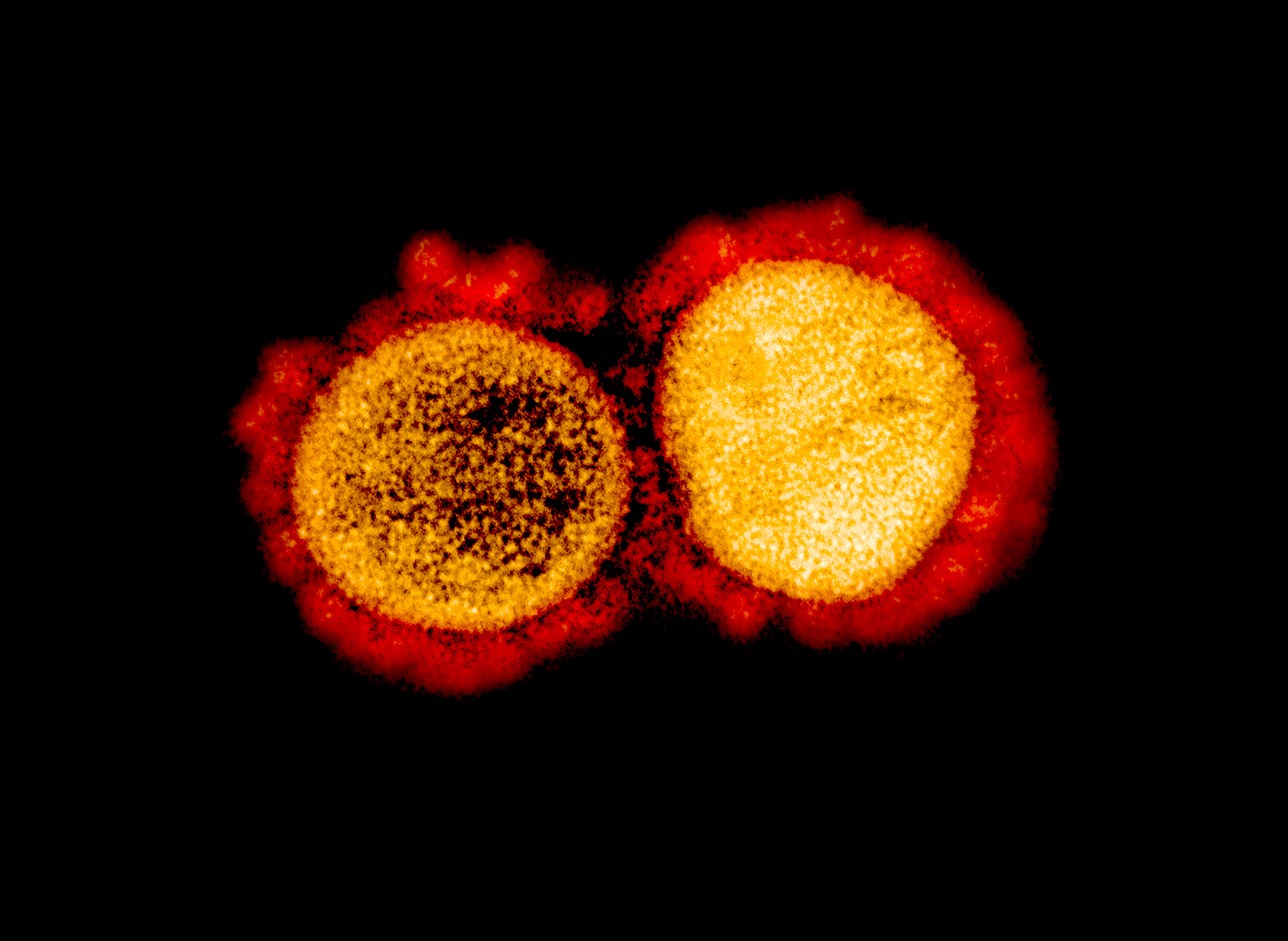
The majority of COVID-19 cases will be mild, however, and many sufferers will recover completely at home. But many of the patients with severe cases who are admitted to hospitals will suffer respiratory failures, according to a retrospective study of patients in Wuhan, China, where the virus originated.
Almost one-third of those patients developed Acute Respiratory Distress Syndrome — a deadly, suffocating condition.
Ventilators are used for patients with dangerously low oxygen levels who cannot breathe on their own. In many cases, patients are sedated and chemically paralyzed so they will not fight the ventilator tube snaking down their tracheas and forcing oxygen into their lungs.
Most patients in their ICU are ventilated, Justine said. But new studies show most patients on ventilators will not survive.
“They’re very, very sick,” she said. “We sedate them, we lay them on their bellies while they have a tube in their mouth to help them breathe. Sometimes we have to paralyze them. Their lungs are so injured that they can’t do the breathing they need to do in order to oxygenate, to get enough oxygen.”
Sarah was shaken from watching a young, fit patient with no preexisting conditions fight to breathe while the virus made the patient’s lungs stiff and crunchy. Marcie said there has been a disturbing number of young people with COVID-19 in the ICU.
That patient fought the ventilator so fiercely that sedation three times the maximum amount typically given to patients was administered, Marcie said. She said it was the most medication she has ever seen delivered at one time.
“The older population don’t have the reserve, don’t have the fight,” Marcie said. “But those younger patients are the ones that are working really hard to stay alive.”
‘Last straw’ treatments tried
Most intubated patients start off lying on their backs, Sarah said. If they max out on the amount of oxygen that can be administered, the patients are flipped onto their stomachs, allowing the lungs to further open up.
It is a strategy that was once reserved for the most severely debilitated patients but is now used regularly to keep patients alive. Nitric oxide can be added to the oxygen as a last resort.
“Those are the last straws,” Sarah said. “We don’t have more straws after that.”
People die from COVID-19 because they cannot get enough oxygen, Sarah said, or because the sedation and lack of oxygen sets off a chain reaction that leads to organ failure. She said the infection can damage lungs so severely that the small amount of oxygen expended by the patients’ bodies when readjusted can cause them to crash.
Even if they survive, the road to recovery for patients is long, Justine said.
“The people that are getting well out of the ICU are going to have months of recovery. Months. They are weak and their lungs will never be the same — ever,” she said.
The traditional treatment plan for intubated patients has been to transition them onto safer, non-invasive devices like BiPAP and CPAP machines, Justine said. These machines put pressure on the lungs, creating a balloon-like effect that makes it easier for patients to inhale and exhale.
But these machines also aersolize the virus, scattering it into the air and increasing the risk of infection. The unit has recently started transitioning intubated COVID-19 patients onto these machines. Justine said it is a positive step for patients — but potentially dangerous for hospital workers not wearing proper protective gear.
“It’s scary, because where do I draw the line of protecting those that are working there and protecting the patients?” she said.
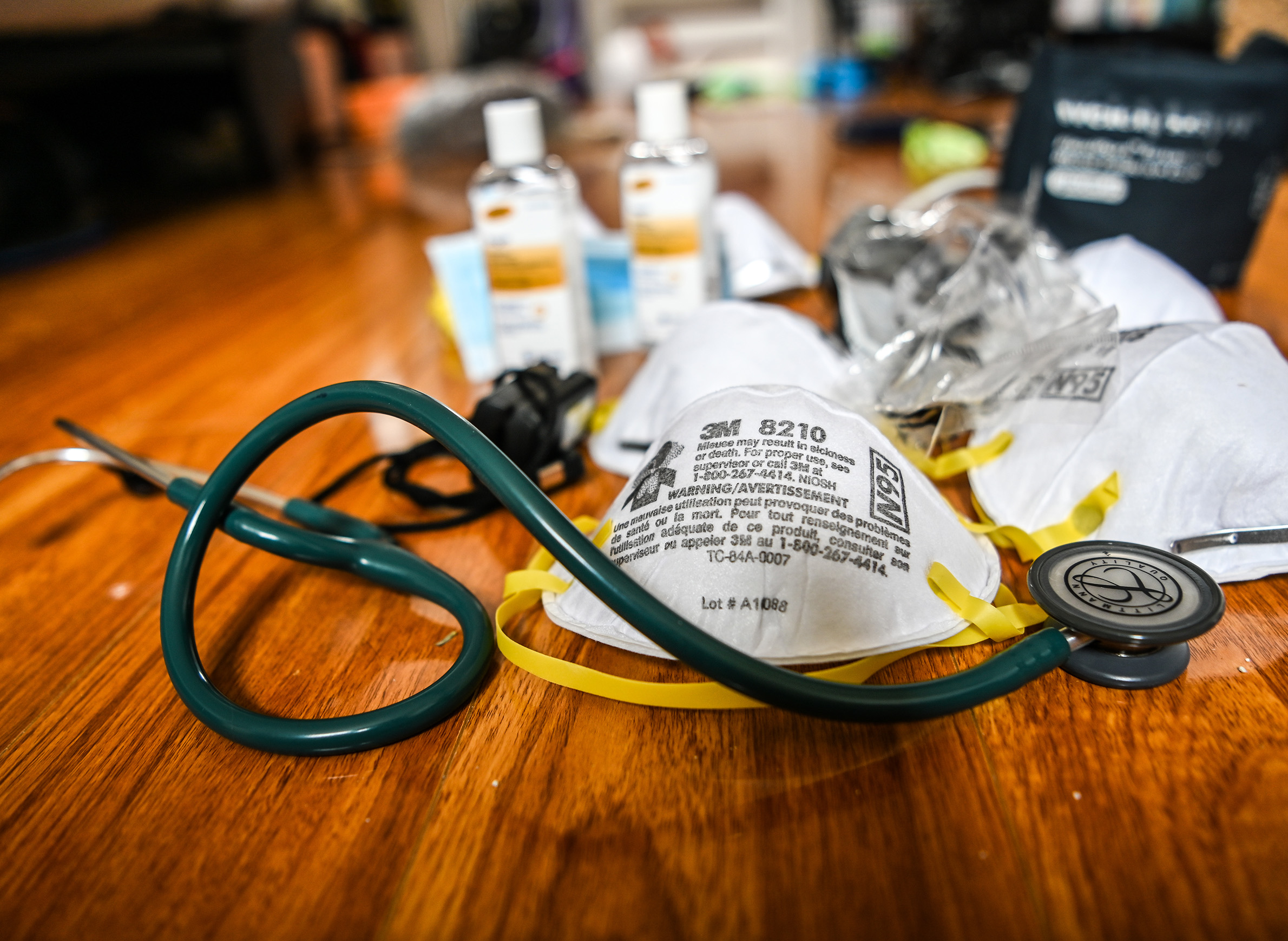
The three nurses said hospital personnel have to reuse N95 masks — sometimes up to three times — before getting a new one. After they finish a shift, the nurses tuck their masks into to-go food containers with holes poked in them so they can air out.
These frontline health care workers have begun buying respirators from hardware stores in case the hospital runs out of masks.
Marcie prefers the powered air purifying respirator, or PAPR, a space helmet-looking contraption that makes her feel less claustrophobic than a tight-fitting N95 mask, which the hospital has begun to have nurses share.
Most nurses in COVID-19 units wear N95s all day — sometimes for 12 hours straight. The masks dig deep grooves into their faces and can cause bloody noses from dryness.
Justine said when a nurse tried to get a replacement for a mask that had been bloodied, the person distributing supplies pushed back, questioning whether it was truly needed. That underscored for Justine the rationing of supplies already underway at the hospital — and what they might face if a surge hits.
Protective equipment falls short
State public health officials have said the shipments of supplies from the Strategic National Stockpile have begun, but they will not be enough to meet demand.
“What we have received from the Strategic National Stockpile barely begins to meet the need or the requests of the Wisconsin health care system,” state Department of Health Services Secretary-designee Andrea Palm said April 6.
Bob Scheuer, director of materials management at UW Health, said the two shipments received from DHS from the stockpile were helpful but a “small fraction” of what the health system actually needs. He was not aware of receiving any other supplies from the state.
The health system has largely had to acquire its own supplies, asking its normal suppliers to step up deliveries and drawing from its emergency supply. Scheuer said UW Health is focusing on acquiring gowns, specific sizes of N95 respirators, PAPR hoods and testing kits — but those supplies are “very, very tight.”
“The need for PPE, especially in a respiratory pandemic, is significant,” he said.
Right now, the hospital group is well-prepared for the projected peak. But “all bets are off if all the predictions are wrong and you double the peak,” he said.
The other hospitals in Madison – UnityPoint Meriter and SSM Health St. Mary’s – did not make supply chain managers available for an interview.
In emails to the Cap Times, a spokesperson for Meriter said hospital officials are “confident in our current supply of PPE and are aggressively working to get more.” A spokesperson for St. Mary’s said “our caregivers have what they need to safely deliver care” but the hospital is “working to conserve supplies, as well as finding new supply sources for certain items.”
The nurses interviewed by the Cap Times and Wisconsin Watch said they feel a disconnect between the messaging of hospital administrators and the rationing of supplies they experience on the frontlines.
“I get that they are trying to save PPE, but they need to protect the people now,” Justine said. “Because if we don’t, and [hospital workers] get sick, then who’s going to take care of the patients that come in in seven to 10 days?”
The lack of protection and potential for infection has at times divided nurses taking care of infected patients from nurses on other units.
Sarah and Marcie recalled a moment when nurses from a non-COVID-19 unit refused to get on an elevator with nurses who had been exposed to the virus. Marcie said she “can’t even express how disgusted and disappointed” she was.
“I never thought it would get to that point,” she said.
‘Beautiful spots of light’
The hospital has adequate staffing at the moment, and nurses said they are able to spend as much time at the bedside as they did before the pandemic struck.
Nurses from other units have been brought to the ICU and given a crash course in critical care nursing — an intense speciality because nurses expect many of their patients to die and must have a plan to stop that from happening.
It’s a type of nursing that can take months to feel comfortable doing, Marcie said. That’s worrisome, Justine added, and it’s personal — one of her family members is hospitalized with COVID-19.
“The standards won’t be the same if we get this surge of patients,” she said.
Hospital staff have to take all of the necessary precautions, even when a patient is crashing, which can feel counterintuitive. Medical workers methodically wash their hands and put on their protective gear as a spotter stands by to make sure everything — gloves, gowns, masks, face shields and hoods — is donned correctly.
“Terrible feeling to watch them crashing, watch their pulse ox[ygen] get to a level that can cause brain damage, and be meticulous about putting PPE on so you can help others,” Marcie said.
The human aspect of nursing is also different. Many patients are unconscious or have so many drugs coursing through their IVs that they are unaware and confused. Staff are covered in so much protective gear that patients see them as a “shapeless being with eyes coming at them,” Justine said. She thinks staff should tape pictures of themselves to their chests so the patients know what they look like.
However, Marcie sees some hope amid the pandemic.
Their unit has regularly gotten donations of food, and the staff are moved by the notes of support written on sidewalks and windows. Marcie said she was teary-eyed when she found notes of encouragement left on all of their cars in the parking garage.
In one interview, Marcie wondered whether the young patient she cared for would survive. A week later, she said the patient was about ready to “fly,” meaning breathing well enough to come off the ventilator.
She said it was “not expected at all, in all of the darkness, to have all of these beautiful spots of light.”
This story was a collaboration between the Cap Times and Wisconsin Watch. The nonprofit Wisconsin Watch collaborates with Wisconsin Public Radio, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.
 Passport
Passport









Follow Us