The Fragility Of Volunteer EMS Systems In Rural Wisconsin
Rural health challenges become even more stark when seconds can make the difference between life and death.
August 28, 2017

HAN: Ambulance exiting garage in Durand

Rural areas in Wisconsin and across the U.S. face an entrenched array of health care challenges, from shortages of primary care and mental health providers to more prevalent cancer risks. These challenges become even more stark when seconds can make the difference between life and death.
According to the Wisconsin Office of Rural Health, 38 percent of Wisconsin’s population lives more than a 10-minute drive from a hospital that can provide emergency care. In large areas of the state, the drive time to an emergency room can exceed 20 minutes or even 30 minutes. Many areas of Wisconsin that are more than a half-hour away from emergency care, particularly in the northern part of the state, correspond with the USDA’s Frontier and Remote Area Codes designation, which is one of several ways to define rurality.
Wisconsin Drive Time to Emergency Care Wisconsin Office of Rural Health July 2017 (Text)
The presence of people trained in first aid, CPR and other life-saving techniques is crucial in rural areas, particularly when they’re volunteers. But volunteer-driven EMT services in rural Wisconsin have had a hard time recruiting lately, with health officials and state legislators questioning the wisdom of relying on volunteer EMTs in the first place.
One community struggling with a shortage of volunteer emergency workers is Durand, a city of just under 2,000 people on the banks of the Chippewa River in Pepin County.
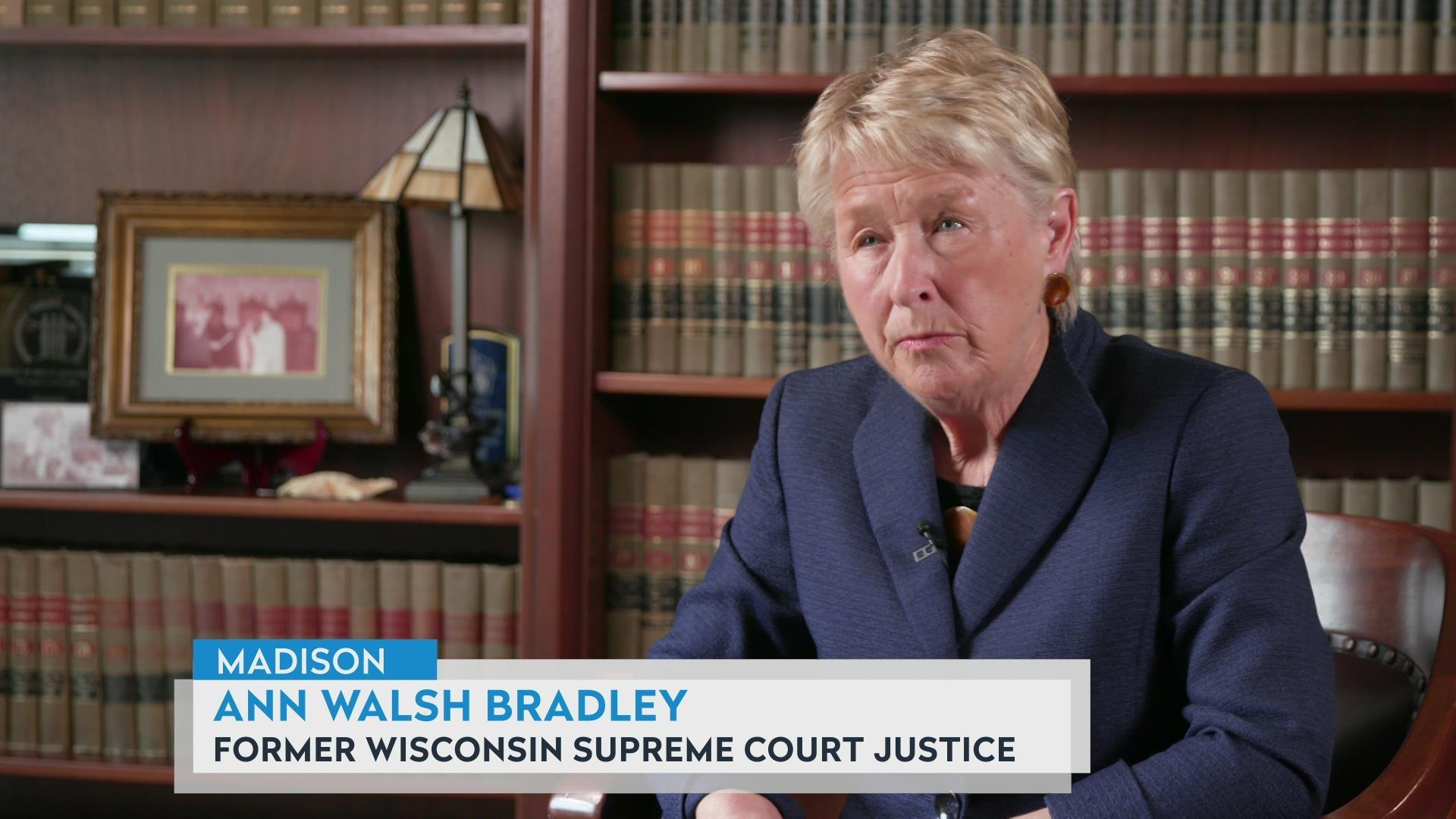
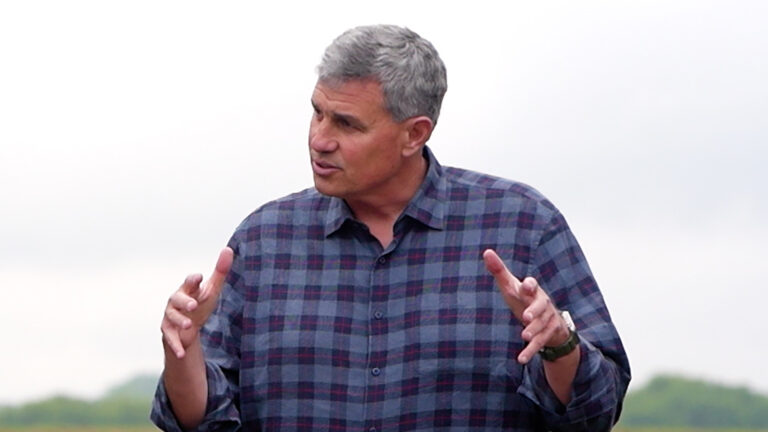
“We have seen a decrease in the number of people that have time or are willing to put time into community involvement, specifically on the ambulance, probably because the commitment is quite extensive,” Durand ambulance director Peter Pillman told Wisconsin Public Television’s Here & Now in an August 25, 2017 report.
Pillman sees a lot of economic strain behind his recruiting problem. Many Pepin County residents commute to jobs in neighboring counties or in Minnesota, making it harder to commit to on-call volunteer work at home, not to mention the required extensive training. Job loss and government budget cuts leave people with less financial security and therefore less free time to volunteer.
Durand still attracts civic-minded volunteer EMTs, and in fact, it’s now offering to pay for their work. But even enthusiastic volunteers or paid employees are likely to eventually move on, sometimes to other careers in the healthcare world. The city’s ambulance service will also need to increase the fees it charges the communities it serves in order to gain new revenues to pay for its new employees.
Pillman has another personal connection to what Here & Now reporter Andy Soth called “the fragility of the system.”
In an incident caught on a security camera, Pillman’s father had a heart attack in a grocery store. A bystander who knew and performed CPR, with help from volunteer EMTs who arrived later, were able to save Pillman’s father’s life. But he was lucky. People who have heart attack under those circumstances — in areas with sparse health care and emergency services — are much less likely to survive than their urban counterparts.
 Passport
Passport









Follow Us