Marisa Wojcik:
Welcome to “Noon Wednesday,” I’m Marisa Wojcik, multimedia journalist with “Here & Now” on PBS Wisconsin. Today is September 1. The city of Madison is launching its unarmed first program called alternative response emergency services to respond to health-related calls instead of the police. Joining us today to explain how it works is Che Stedman, chief assistant of the medical affairs with the Madison fire department. Thank you so much for being here today.
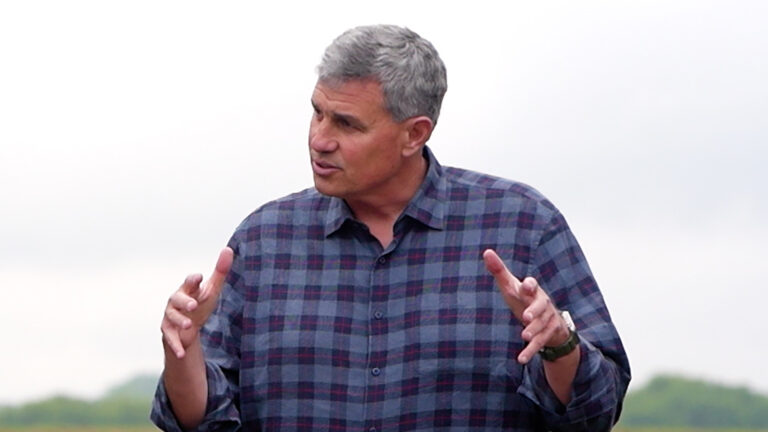
Ch Stedman:
Happy to be here.
Marisa Wojcik:
Just to start, how does this new program embedded within the fire department instead of law enforcement work?
Ch Stedman:
Yeah. So, it is a 911 service, so any EMS, law enforcement, or fire related calls that come through 911 all get triaged to the appropriate resource, right, as that system works. This is just an extra resource, and this particular team has a community paramedic from the fire department and a crisis worker from Journey Mental Health that can respond to nonviolent behavior health related emergencies coming through the 911 center.
Marisa Wojcik:
And so how do you decide if a call is answered by this team or by police, especially if time is of the essence?
Ch Stedman:
Yeah. So, the 911 dispatchers and the call takers in the 911 center are really integral to this and have done a lot of training around it. This is something they have already done. They are very aware of the questions they need to ask the people that are calling 911 and to send the right resource. They have done that for decades and decades. Now they just have to make sure this team follows a particular set of protocol questions, such as, you know, with the behavioral health emergency going on, is there any danger involved? Weaponed involved? Somebody on scene being violent? If any of the questions are answered to the necessity of having law enforcement there because of some sort of violent situation going on, then law enforcement will still be sent in first to make sure that scene is safe. If the information from the 911 caller is that, yes, this is a, you know, a safe situation, but there is somebody having a behavioral health emergency, then they just send the crisis response team, or CARES team, directly to the scene. The 911 center is a very important partner in this, and it is really them still doing the same job they’ve always done with just extra resources available to them.
Marisa Wojcik:
And what exactly are the first responders, this team of two, doing when they respond to a scene?
Ch Stedman:
Yeah. So, fortunately, the information from the 911 center and the questions we’re asked there all get loaded into a computer aided dispatch system, and so all of that information shows up on a computer that the responders have available to them so they can kind of see what the information is, kind of know what they are walking into, and their job really is to initially deescalate the situation and make sure that they provide an appropriate intervention, and whether that’s a behavioral health intervention on the part of the journey crisis worker or some sort of medical assessment by the medical paramedic, those folks at the scene can make the decision, which protocols to follow, which intervention is most appropriate, and most importantly, with programs like this around the country, we find people in some sort of mental health crisis or behavioral health crisis, they tend to not want to see folks walking in with guns, right, and so no matter how good law enforcement is at their job, no matter how good they are at deescalating the scene, just the presence of somebody in a uniform and a gun on them can exacerbate the situation. So our responders that come into any situation are not in formal uniforms, not responding in lights and sirens and a big fire truck. We hope initial de-escalation is possible. After this, it is about providing the appropriate intervention core with the person at that time, and even then, referring them to the appropriate mental health resources within the community so we can work with them on scene but also drive them to the appropriate facility specific to their needs.
Marisa Wojcik:
And so, if it is needed, will there be a possibility of, in some cases, officers intervening after the team of two of mental health responders get to the scene and maybe things change?
Ch Stedman:
Yeah. Certainly. If they are unable to deescalate the situation or any sense there is something illegal going on, then, of course, law enforcement resources would need to be brought in, but the intent of the team is to not have these people that we consider to be patients, right, that need more help on the medical side of behavioral health side and hopefully keeping them out of the law enforcement world in general, if they are not needed there. These folks don’t need to be contacted and set down a path towards jail when the path really that’s going to help them is towards a mental health intervention so at any point, a law enforcement office can call this team and have them come in. This team can call law enforcement, have them come in, and it is the same on the medical side. If the paramedics are visiting with somebody who doesn’t have an acute medical problem, but they have something more low-level that’s also a behavioral health issue, the paramedics in the field can call the CARES team to come in and make that intervention so that the person can have a continuum of care that’s better than the paramedics saying, well, you don’t need a transport to the hospital, we are leaving, good-bye, have a good day, right? We offer this extra care that takes the person downstream and gives them a warm handoff to the appropriate mental health provider and have that referral take the person to where they need to be.
Marisa Wojcik:
What was the impetus of bringing this to Madison, and is the model youre implementing based on programs already put into practice in other cities?
Ch Stedman:
Yeah, great question. So, we’ve been looking at the other models here at the fire department for a good four or five years. Specifically, the models we researched the most was in Eugene, Oregon and the Star program in Denver. There’s quite a few around the country as well operating successfully so the impetus was although we know the programs are effective, we finally got money in the budget this last year. One of our city alders, Alder <artin, was big in the initial start, talking with Fore Chief Steve Davis last year, and support from the mayor’s office and common council, and they were able to budget approximately half a million dollars for the team annually, and the hope and vision of the team is they will be able to grow. Right now, our little pilot program that we’re running is just being run in the central police distribute of the city of Madison from the Ohara river to Park street, and we are only running it Monday through Friday from 11:00 a.m. to 7:00 p.m. and so the vision is to have a team that works 24/7 throughout the whole city and eventually, hopefully, the whole county, but, yes, researching other programs were key and give us good information about the right things to do, thing we shouldn’t do, how to evaluate the program over time using data, and so the other programs successful out there have been a great help.
Marisa Wojcik:
City data says that Madison receives roughly 7,000 mental health related calls per year, 20 calls per day, and primarily answered by law enforcement. Would this program be aimed at alleviating some of that stress on law enforcement, and is it also meant to prevent unnecessary injury or death to someone who needs mental health services by a police officer, as we have seen in a lot of media reports over the last year and a half.
Ch Stedman:
Yeah. So there’s certainly going to be a reduction in stress on law enforcement because of this, and that’s kind of a side effect of us taking over some of these calls for them, and so the hope is that, you know, if we look at harm reduction studies and the right path for people, we hope to, you know, divert people from the criminal justice system and hope to divert people to emergency rooms too because the hospital emergency rooms can become overwhelmed with folks who don’t necessarily need emergency room services, and so, you know, we are looking at just making our whole 911 system more appropriate. It relieves stress on the folks who don’t need to be a part of the situation, and, really, we want to be patient centered. We want to do what’s right, provide the right intervention at the right time for folks in behavior health crisis that don’t need law enforcement and don’t need emergency help.
Marisa Wojcik:
How is this different from crisis intervention teams or having mental health specialists that are part of law enforcement teams?
Ch Stedman:
Yeah. It is similar. The big key here is that we are trying to bring a team that doesn’t have a law enforcement officer, and so we have a lot of questions around safety. You know, is this team going to be safe? You know, how can you assure their safety? The fire department, in general, responds to a lot of calls on our own, and when we come to a scene and we recognize an element of danger or weather its a weapon or anything else, we are trained to deescalate as best we can out of the scene and call for law enforcement backup. That’s how the team is trained. That’s why there’s a fire paramedic personnel on the team so they can kind of keep that umbrella of safety around the team when needed, but looking, again, at the other programs around the country, we find when the 911 center does the job appropriately and sending the team into a situation that is safe as they can tell that it is through the 911 call, that doing this without law enforcement should be a good model, but we always have that law enforcement backup if needed, and because that fire department paramedic is there, their radio and safety training they have and de-escalation training, we expect that this team will hopefully be safe, and be able to operate in a manner that will really, truly help our patients.
Marisa Wojcik:
While you helped to work implement this program, what did you hear from public input, and how is it specifically tailored to the Madison area and Madison needs?
Ch Stedman:
Great question. We did quite a few listening sessions. We talked with not only community members, but mental health providers in the area, and we talked with the University of Wisconsin Mental Health Services because they are kind of in our jury diction as well. We spent the few months before we went live really getting out and talking with folks about what the needs of community are and what best practices were according to providers, and, you know, every state and every city has different state statutes and ordinances, and so there are things done in Eugene, Oregon that we can’t do here. For instance, around emergency detentions and something law enforcement has to be involved with in the state of Wisconsin by statute. If somebody needed to be put in custody and protective custody under emergency detention, we have to have a law enforcement officer on scene. The great thing about the city of Madison and Dane County in general is that we have a lot of resources. You know, social services are strong here. The one thing we are mostly hopeful about is that we really believe we’re going to be able to take the situations that we encounter and connect those folks with some sort of service that’s going to be appropriate for them, and, you know, we were very thoughtful in making sure that our team was diverse. We actually extended out our hiring process for the community paramedics because we wanted to see, hopefully, people of color applying, and we were fortunate in getting bilingual Spanish speaker as one of our community paramedics, and both of the Journey Crisis Workers identify as people of color, and so that was very important to us to make sure that, you know, we had a team that represented the community, that was some of the feedback that we had gotten, and other feedback from the community was don’t show up with badges and uniforms on looking intimidating, so we decided to put them in civilian-type clothing, and we gave them a lot of de-escalation training, a lot of extra crisis response training that community paramedics needed. As 911 paramedics, we don’t have training around mental health response in the basic paramedic class, so we sent them to a 40-hour class, crisis intervention training that is a nationally certified course and sent them for de-escalation training and motivational training, and others designed specifically around mental health, and the journey crisis workers are masters and bring a lot of the expertise to the team as well. Depending on what county and what state you’re in, teams may look different, but we did our best to model ourselves over those best practices.
Marisa Wojcik:
Sometimes people don’t want to call police officers in a certain situation fearing the ramifications of making that call. Will this encourage people to reach out for emergency assistance that might not normally otherwise?
Ch Stedman:
I sure hope so. You know, we have done our best to get the information out there about this team. If folks are nervous about calling 911 because of the possibility of law enforcement showing up at their home, that’s unfortunate. I personally, you know, have worked with our police department here in Madison for 25 years and have faith they do the right thing, and they have been specially trained to handle mental health calls, but I certainly understand why folks don’t like somebody wearing a gun walking through their door in these situations, and so, you know, I hope that as this team shows success over the next few months and we collect data showing that patient satisfaction is there and we’re really helping people, we’ll get more funding to expand the team out and provide these services to the entirety of Dane County and the more this team responds to the behavioral health crisis and keep law enforcement doing the things they need to do on the law side of things, I think it’ll just work out best for everybody in the community.
Marisa Wojcik:
Now, it’s worth noting today is the first day of the pilot program, so what are your short-term goals, long-term goals, and how are you measuring success?
Ch Stedman:
Yeah. Great question. Yes. You timed this interview very good today. We just started at 11:00 a.m. today for the very first day. So, the measuring success is a tough one. It depends on who you ask, right? If we’re being as patient centered as possible, it is about getting patient satisfaction surveys and following people downstream through the referral to make sure they engage in the services. When we looked at the evaluation criteria from the other successful teams, it was things like a fewer calls to that the police department responded to, a fewer people sent to emergency rooms and jails because of crisis responses, and most importantly, patient satisfaction around the treatment they received so we have data analyst assigned to us from the city of Madison that’s pulling all patient care reports both from Journey Mental Health and the fire department looking at all the data, accumulating everything they can get together and present that to the mayor’s office and public health and to have them evaluate it and let us know if we should shift directions or not. Short term, my goal is to keep our teams safe, keep them responding in helping people, and long term it’s going to be likely fighting for money to expand our team.
Marisa Wojcik:
All right. We leave it there, Che Stedman, Assistant Chief of Medical Affairs with the city of Madison Fire Department, thank you, good luck with your first day, and keep going, and thank you for your work and thank you so much for joining us.
Ch Stedman:
Thank you very much, I appreciate it.
Marisa Wojcik:
For more from “Here & Now” and PBS Wisconsin, you can visit pbswisconsin.org/news, and thank you so much for joining us on “Noon Wednesday.”
Search Episodes

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport












Follow Us