Marisa Wojcik:
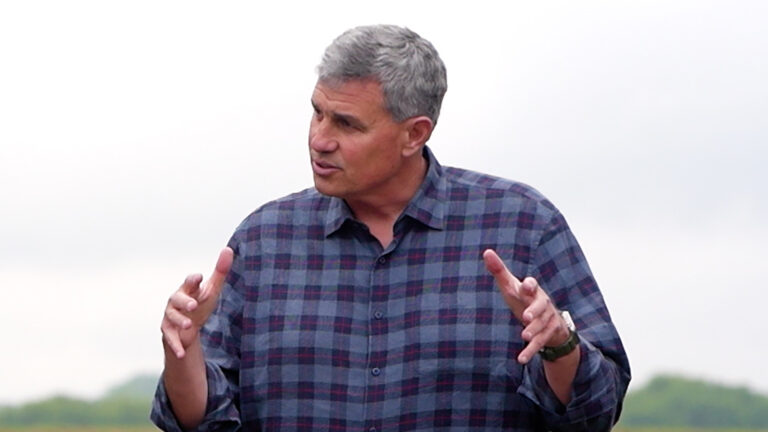
Welcome to Noon Wednesday. I’m Marisa Wojcik, a multimedia journalist with Here & Now on PBS Wisconsin. Today is May 27th. What was expected to be a surge of COVID-19 patients overwhelming Wisconsin hospitals didn’t materialize like it did in many other parts of the country. And now, Wisconsin is reopening. Measures to slowly turn the dial are getting the green light. So what does that mean for hospitals and health care workers going forward? Joining me today is Dr. Mark Kaufman. He’s the Chief Medical Officer from the Wisconsin Hospital Association, and Dr. Kaufman, thank you so much for being here.
Mark Kaufman:
Thank you for having me, Marisa.
Marisa Wojcik:
So the governor’s Badger Bounce Back plan included metrics and gating criteria specifically aimed at Wisconsin hospitals. What did that include?
Mark Kaufman:
Well, there are a number of metrics. Most of those had to do with what are called crisis standards of care, and that’s the ability of hospitals to operate not under very specific crisis standards of care. And I believe the BBB metrics had to do with the percent of hospitals that were able to do so. And actually, since the Department of Health Services has been reporting that metric, greater than 95% and typically 100% of hospitals have been able to operate under non-crisis standards of care. And I think the other metric had to do with the trend in the number of health care workers who came down with COVID-19.
Marisa Wojcik:
And did any Wisconsin hospitals kind of reach their maximum capacity in the last three months?
Mark Kaufman:
So I think you’re probably referring to sort of the ability to take care of very sick patients with COVID-19. And typically, when people ask that question, it’s about the number of beds, the number of ventilators, the number of ICU beds. And the answer is no, that I’m aware of. No single Wisconsin hospital really reached that, and that was for a number of reasons. The first is, is that all hospitals cut back on elective, even though they were necessary procedures and they would help patients, they really decided to cut back to create additional capacity in all those resources, so if the initial surge or wave of patients very ill with COVID-19 who needed to be in the hospital was really large and really sudden, the hospital would be able to provide the necessary resources. That huge surge never happened, a lot due to the good behavior of Wisconsin citizens in terms of physical distancing, staying at home, being safer at home. So because of really a number of reasons, no hospital really was overwhelmed. Typically what people think of, the views in the news of what happened in New York hospitals with terrible, terrible situations of EDs crowded with very, very ill patients, that did not happen in Wisconsin.
Marisa Wojcik:
So prior to this pandemic, a lot of hospitals have been trending towards a leaner staffing model. For the last three months, what did staffing at Wisconsin hospitals look like if we were preparing for a surge that never happened, but we were trying to get ready for it?
Mark Kaufman:
Well, I think most hospitals tried to right staff. So what that means is when, before the initial surge, when nobody knew how it was going to be, hospitals really cut back on procedures, and they also cut back on what their staff were doing ’cause they weren’t doing their normal thing. The other issue about cutting back on procedures is preserving the supply of personal protective equipment, which hospital health care workers really need to protect themselves while taking care of COVID-19 patients. So before that initial surge, which was predicted about the middle of April, hospitals were watching the data, they were preserving their PPE, they were trying to keep their health care workforce in reserve and safe. Now that we’ve at least weathered the initial surge without overwhelming any of the hospitals, hospitals are beginning to reschedule delayed and postponed and necessary procedures which patients really need to be healthy and to stay healthy. So now there’s more health care workforce engaging in patient care at hospitals as hospitals gradually ramp up to take care of the patients that they need to.
Marisa Wojcik:
And I did want to ask you about procedures as we’re opening back up. So it’s not going to be, the floodgates are just open, It’s a slow process of more and more surgeries and procedures being allowed to happen. Will that get back to full capacity?
Mark Kaufman:
Well, we will see, but you’re correct. That is what happened. And in many hospitals, what happens is a group of clinicians and other people get together, look at all the postponed and canceled surgeries, and because they’re going to restart gradually, what they do is they prioritize the procedures that are most urgent to get done to preserve patients’ health. At the same time as they gradually ramp up, everybody is keeping an eye on the number of COVID-19 infected patients in their area, the critical hospital resources in case there’s a spike or a second wave or a surge, personal protective equipment. They’re always trying to balance the needs of the patients that they have that don’t have COVID-19, gradually open up and take care of those patients, but always with an eye on what could happen if there’s a second wave or surge, and again, managing that so they’re not overwhelmed and we can take care of those patients.
Marisa Wojcik:
Your organization came out with a press release saying that anecdotally, you’ve been hearing patients are nervous to even get emergency care because they think going to the hospital, they’re going to contract COVID-19. What’s your response to that?
Mark Kaufman:
Well, it’s ironic, because hospitals of all institutions, are the safest places, who are the most experienced at infection control, you know, beyond COVID-19. Infections are everywhere, and hospitals always have to deal with keeping people safe. The fear is understandable, people watching the news. There’s good data from other states, from a Kaiser study in northern California, where patients clearly delayed emergency care, the mortality rates were beyond in New York as they looked at that. The mortality rates for other diseases were much greater in terms of heart disease and stroke, ’cause many patients decided to not go to the hospital because of that fear. I think that fear is really unfounded. I mean, hospitals truly are expert at infection control, at segregating infected patients from noninfected patients. Their cleaning procedures have been really ramped up, above and beyond. While the fear is emotional and understandable, you know, it’s really from a scientific standpoint, unfounded. But we all have to deal with that and manage that, and make patients and staff feel comfortable ’cause it’s a real dynamic out there.
Marisa Wojcik:
And part of that infection control, as you mentioned, is managing PPE. As it stands– PPE, which stands for personal protective equipment, as it stands right now, what does that inventory look like for Wisconsin hospitals all across the state?
Mark Kaufman:
So, much better than it did four to six weeks ago. It’s not really what it was, let’s say two years ago, but there’s been a lot of innovation. The CDC has guidelines for the appropriate reuse of personal protective equipment. Other suppliers have come to the fore, Wisconsin companies. There’s been innovation in terms of reusing PPE and sterilizing it. The state of Wisconsin has been involved with that in terms of using UV light. I think the biggest mild shortage right now are surgical gowns and what are called N95 respirator masks, which are what health care workers use and really can filter out very small particles, including viruses. But in general, the PPE supply at Wisconsin hospitals is much better, the supply chain is much sturdier than it was six or eight weeks ago.
Marisa Wojcik:
And with PPE and ventilators, if more people started to get sick, would we have the capacity now to be prepared for a surge that hasn’t happened yet?
Mark Kaufman:
Well, if you actually look at the ventilator capacity in Wisconsin, and on the WHA website actually there’s a daily refresh of ventilator capacity. As of this morning actually, there were about 318 ventilators in use across all Wisconsin hospitals for all patients, just not COVID-19, and a total of about almost 1,300 ventilators. So really, 25% utilization of ventilators. So even though the concern was ventilators, it’s never been realized. And ventilator capacity for the last three months has always been really large to absorb a surge of very ill patients. As I said, PPE is a lot better, and again, as hospitals reopen and start to reschedule postponed and necessary surgeries, one of the things they keep their eyes on are the supplies of PPE. And they’re always trying to appropriately balance the PPE that’s needed to take care of rescheduling of these delayed surgeries, and how much they will need to keep in reserve if there is a spike or a secondary wave of critically ill patients with COVID-19.
Marisa Wojcik:
I did want to ask you, are you expecting a second wave, and are you advising your hospitals to be prepared for a second wave? What does that look like?
Mark Kaufman:
Well, I think all hospitals are following the data on a daily basis. And if you look at the number of patients in the hospital, diagnosed with COVID-19 all across Wisconsin on a daily basis and you look at that trend over time, there has been a slow but sustained increase over the last three weeks. Despite that increase, when you look at ICU bed availability, ventilators availability, staff availability, regular bed availability, there’s plenty, there’s plenty of staff, supplies, and stuff, is what we call that. But we all are aware that as Wisconsin citizens become less homebound, as businesses open up and people come closer together, we all realize that there is likely to be more cases of COVID-19. Hopefully though, with our increased testing capacity and hopefully an enhanced contact tracing capacity of recently diagnosed patients, if there is a bit of a spike or a surge, we can quickly identify where that is, find the contacts, isolate those people, test those people, and contain a focal spike from becoming a big wave that rolls across the state.
Marisa Wojcik:
With increased testing, you’re now… We’re no longer only testing people with critical symptoms. So with increased testing, some people, the data is showing people testing positive even they were asymptomatic. Is it tough to look at the data and understand a true picture of who might need critical care?
Mark Kaufman:
So it’s not hard to figure out who might need critical care, ’cause those patients end up in the emergency room and they present with, in dire medical straits, right? But I think to the first part of your question, because we’re really increasing our testing capacity, and we’ve moved from testing patients mostly in the hospital very ill with COVID-19 symptoms, to now, really anybody with a cold as an outpatient. We’re going to find many more patients who have COVID-19 because we know that 50-80% of the people who get COVID-19 are minimally or asymptomatic. So when you look at the testing numbers go up, the number of cases will go up. But what won’t be impacted by the availability of testing or the expansion of testing criteria will be the number of critically ill patients, because whether they’ve been tested as outpatients or not, they’re going to end up likely in the emergency room, in the hospital. So what a lot of us follow, really, is the pattern of hospitalizations. And looking at the number of people in the hospital with COVID-19, that has really very little to do with testing except if you get tested in the hospital. But if the number of people in the hospital with COVID-19 is just gradually going down, down, down, down, that is a sign that the pace of the spread of the pandemic in Wisconsin is decreasing. If the slope of that line is gradually increasing, which it has been over the last three weeks, to me what that says is, is that the rate of the spread is gradually increasing. And what’s really interesting in the last week, at the same time we’ve seen a gradual three-week increase in the number of patients in the hospital with COVID-19, in the last seven days actually, despite doing more testing, we’re seeing a decrease in the number of patients with confirmed cases. Now what you have to realize is, is that if patients are going to get very ill with COVID-19 and need a hospital bed and hospital care, there’s usually a two or two-and-a-half-week lag from them becoming exposed to COVID-19 to needing a hospital bed. So the hospitalization is sort of a lagging indicator by about two weeks of what’s happening in terms of spread.
Marisa Wojcik:
And so now that the entire state is back open, you know, the initial wave we saw a concentration of cases in certain parts of the state. Are other parts of the state going to need to be more careful, and are those hospitals going to be planning differently between urban and rural and different populations?
Mark Kaufman:
I think we’re all going to need to be more careful, regardless of where the hospital is. In the last three weeks, the number of patients hospitalized has gradually risen, mostly in south central Wisconsin, southeastern Wisconsin, and the Fox Valley. Three or four weeks ago, there was a spike in the Green Bay area related, I think, to meatpacking, locational exposure. But really, the pandemic’s going to spread throughout Wisconsin. It’s going to be impacted by the current prevalence of infected people, how people maintain physical distancing, whether they mask or not. And then in terms of how individual hospitals are impacted, it really depends. So you know, the nature of the spread of COVID-19 in rural areas is much less in terms of prevalence, the number of infections per 1,000 residents. But then again, the hospitals are much smaller, you know, with fewer ventilators and smaller ICU capacity. I think the good news is we’re very organized in Wisconsin in terms of the hospital association, in terms of large health systems. We have a lot of good data. Using Milwaukee as an example, the normally competing health systems there, the five big health systems that compete for business have been a model of cooperation in terms of sharing resources, looking at staffing, sharing data, making plans to move staff or resources to a different system if that were needed by the clinical characteristics. So I think we’re all in this together as a hospital, as hospitals in Wisconsin, and the degree of collaboration and cooperation and planning is unprecedented in my 40 years of experience in Wisconsin as a physician.
Marisa Wojcik:
All right, Dr. Mark Kaufman, Chief Medical Officer from the Wisconsin Hospital Association. Thank you very, very much for joining us.
Mark Kaufman:
Thank you, Marisa. Take care, be safe.
Marisa Wojcik:
For more from Here & Now and PBS Wisconsin, you can go to pbswisconsin.org, and thank you so much for joining us on Noon Wednesday.
Search Episodes
News Stories from PBS Wisconsin

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport















Follow Us