Marisa Wojcik:
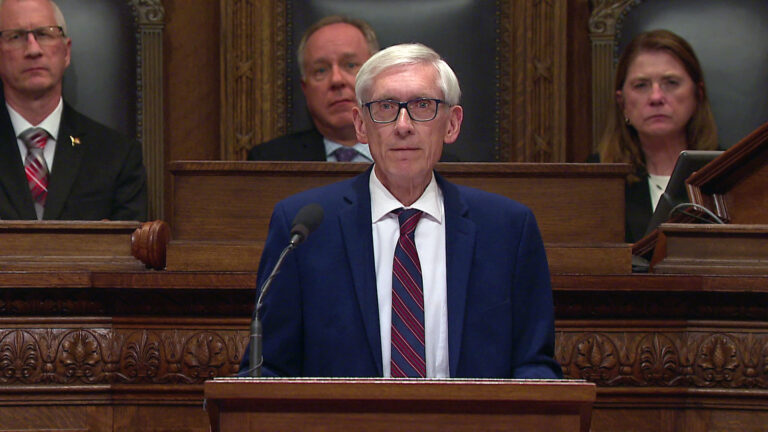
Welcome to “Noon Wednesday.” It’s March 18th, and I’m joining you from a much different location here. We are taking extra precautions in light of the increasing spread of the novel Coronavirus. So, I’m here in our studio by myself. The number of confirmed cases of COVID-19 in Wisconsin have hit 72 and that is with the caveat of testing is still limited in the state. State officials are working on ramping that up, but this is just the number of cases confirmed that we know of based on available testing. Governor Tony Evers and the Department of Health Services yesterday closed all bars and restaurants with the exception of food carry-out and there is a statewide ban on gatherings of 10 or more people, and there are some exceptions like grocery stores and hospitals. A full list of those exceptions are on the Governor’s website. Yesterday, state health officials spoke to the reality that hospitals are gearing up for a surge of new patients as the symptoms of COVID-19 are increasing hospitalizations in countries where the disease has spread further. So, joining me today is Kate Walton, an emergency room nurse at UW Hospital in Madison and joining me remotely from their home. Kate, thank you so much for being here.
Kate Walton:
Thank you so much for having me.
Marisa Wojcik:
I want to start– you’ve been self-quarantine, self-quarantining at home since you last worked. When was your last shift and what was happening at the time that you were last working?
Kate Walton:
I last worked on Thursday of last week, and it was a fairly busy day, made a little bit more complicated by the fact that we had a few patients that were being tested at the time. None of them are my patients. I don’t you know, I don’t know what those results were, don’t really know any specifics about any of those patients, but I do know that that just sort of adds to an extra strain on the department because it means that we have to clean those rooms specially. They have to be left alone for a couple of hours and closed down basically before we could use them again, and clean them fully, and then, it’s a very thorough cleaning process. I mean, we always clean things very thoroughly in the hospital for obvious reasons, but it’s even more complicated and time-intensive so…
Marisa Wojcik:
And, you know, usually a week is not that much of a difference from working one shift to the next, but in this case it is. Have you heard much from your colleagues that have been working since your last shift?
Kate Walton:
A little bit. The– there’s a lot of focus on preparedness right now. So, understanding what resources are there and trying to figure out what adaptations need to be made. So, things are preceding at pace, last I heard.
Marisa Wojcik:
What does that preparation look like?
Kate Walton:
It depends. There’s certain things that, you know, as far as like isolation, for instance, for patients that you suspect may have Coronavirus or COVID-19, that we’re still– we’re fairly sure that we know that it’s transmissible by droplets, things that you cough or sneeze, you know, so making sure that– but it may be airborne in some cases. We’re still, you know, sorting some of that out and assuming that it is until proven otherwise and also that those droplets then, if they come in contact with anything, can be highly contagious, as well. So there’s just a lot of planning as far as where we put these patients so that they don’t infect other patients, how we transport them through the hospital, how we clean things, even, you know, what, if there’s any specific measures that need to be taken for cleaning for this compared to other diseases and other infectious agents.
Marisa Wojcik:
And on a media call yesterday, state health officials said that they’re preparing for a surge. They used the word “surge.” Is that something that is top of mind for hospitals and health facilities?
Kate Walton:
It is, and I mean, that’s why we’re asking everybody to do social distancing right now. So, this is something that, you know, it’s called a novel virus because it’s something that no one’s been exposed to before which means that it’s very infectious. We don’t have antibodies to fight it so we’re concerned that if people don’t practice social distancing that the spread of this could happen much more quickly and that then we might see a surge of cases in the hospital, overwhelming our needs. So we’re just taking measures in the hospital to prepare for that and to figure out what we can do to mitigate that and to also be prepared for that. But we’re also really encouraging people to stay home as much as possible, to work from home as much as possible, and to maintain good social distancing practices, and good, you know, hygiene, like washing your hands.
Marisa Wojcik:
And they did say in that meeting yesterday that those measures are meant to protect the health care system. What has the hospital been telling you or what have you been preparing to expect in the next days, weeks, or months?
Kate Walton:
That, honestly, really depends on how well everyone practices social distancing. So, if everybody, you know, if we do a good job of maintaining that distance and not spreading this disease quickly that may put, you know– You’ve probably heard about flattening the curve. So, we’re trying to keep that surge from happening all at once. We’re trying to see cases spread out more over the next several weeks or months even, sort of, the longer that we can put this off, the better, and if we can get to a point where we don’t see new infections happening in a rapid rate, then we’ll be better equipped and better able to handle any patients that we get. So, you know, right now we’re well-equipped to handle critical patients of any kind. It’s just really a matter of numbers. So, that’s what we’re really encouraging people to follow the rules and stay home and not go out. That’s why I’m really glad to see that, you know, schools are canceled and gatherings of more than 10 people have been canceled or prohibited, and, you know, same with the restaurants and that just the more that we can practice this social distancing, the better.
Marisa Wojcik:
So at the moment the hospitals and health care facilities aren’t looking overrun, but there’s potentially kind of a calm before a potential storm so to speak?
Kate Walton:
Right, that’s my understanding and– Again, I haven’t been at work, but, you know it, it sounds like that right now we’re very much in the preparation stage.
Marisa Wojcik:
How is the hospital ensuring that health care workers themselves are not getting sick?
Kate Walton:
There’s– we always have protective equipment so and there’s policies in place and that’s, you know, there’s trainings that have been offered and again, I can’t really speak exactly to what my hospitals done ’cause I haven’t been there for the last few days, but I know that there’s videos that have been online and some hospitals I’ve seen have done like, basically, partner-based practice where you and a partner help each other put your protective gear on and make sure you’re doing it right to make sure you don’t contaminate yourself. And then, I know my hospital and most hospitals are having workers take their temperature every day right before their shift and maybe multiple times throughout the day, and then any new symptoms they’re having that could possibly be Coronavirus, that those staff are then expected to stay home for a certain amount of time until they’re either cleared by employee health or their symptoms improved.
Marisa Wojcik:
Are you allowed to get tested If you have, if you suspect that you have contracted the infection?
Kate Walton:
I honestly don’t know the specific rules for that. I know overall, and this is true nationwide, that the testing has been very limited. I don’t know the current set of guidelines for testing patients so I’m not really sure if you need a known exposure or not. I do know my hospital is keeping track of who has come into contact with patients that they suspect to have Coronavirus. I don’t know– you know, and then having those staff members monitor, monitor their temperature and monitor for symptoms and report to employee health with that, but I don’t– as to that I can’t really say.
Marisa Wojcik:
You mentioned personal protective equipment. What does that look like and is there is there enough to keep hospital workers safe?
Kate Walton:
We–the equipment that we generally wear is a N95 mask, which is a mask that’s designed to keep airborne particles out. There’s also usually a face shield, Again, with those droplets from a cough or a sneeze, you don’t want those getting to your eyes so we’re taking precautions to cover the face, as well as to protect the airway and then, wearing a gown. I do know that a lot of places are doing– are basically, have looked to see what the most effective way to conserve protective PPE is. So, washing things that can be washed. Using them, you know, there’s certain things that you can wash it with bleach wipes and then use it in different rooms as long as you wash it thoroughly in between much like my stethoscope, right? I wash it between patients, and then can listen to, you know, use it with two different patients, but then there’s other things like masks that can’t be rewashed, you know. So, just trying to conserve that and be good stewards. Use it in cases where it’s warranted, but not use it in cases where it’s not so you know in the hospital. We don’t want visitors who aren’t sick to wear masks, for instance, because it’s not like a mask protects other people from getting the illness that you have so we’re trying to conserve protective equipment in that way and the same with staff, right? We don’t want staff members just routinely wearing a mask if they’re not ill, if they’re not going into a room of a patient that may be ill.
Marisa Wojcik:
If workers are becoming sick, is there, are there staffing concerns?
Kate Walton:
There are. You know, and I think that this is something that we’ve seen across health care that over the last few years especially, there’s been a push to move towards, like, a lean staffing model or so called “staffing matrices” where staff has been cut or reshaped to fit certain projected needs rather than actual needs. So, you know the biggest concern really that we have is that with these cuts that have been, lately, to staff to just enough staff rather than just enough staff, plus more to handle what might also come in the door. So, we’re already a little bit behind in that regard that we’ve, over the last few years, seeing these changes take place in health care, where we’ve gone to this more austerity model and now we find ourselves in the face of something that’s really, fairly concerning and it’s going to take a lot of resources. You know, even with everyone practicing good social distancing and quarantine that we still expect to see a lot of cases of a lot of people being very ill, taking a lot of resources, and the concern there is that on top of that, with health care staffing and the hospital staff– not just the nurses and doctors, but also the people cleaning their rooms and serving the food– that if those staff get sick and we’re already in these sort of austerity measures where we’ve got just enough staff, that it’s going to be harder to fill those holes. It’s going to be harder to provide the care that we’d like to provide so it’s been a concern already. And it’s really just sort of being highlighted by this pandemic right now.
Marisa Wojcik:
Have you been told that your shifts might be getting longer? How long is a typical shift?
Kate Walton:
A typical shift in the hospital is 12 hours. There are some nurses that work eight. Twelve is usually the maximum, although you can work as much as 16 hours, but that’s– usually 12 hours is an average shift in the hospital at least. I haven’t heard anything specifically, but I do know that just as health care workers we’re, you know, trained and we also expect not to leave our patients in the lurch, right. We don’t want to abandon our patients when they’re sick. So, nothing has– that I’ve seen officially, has said that we will have to work longer, but I do imagine that there will be a lot of people that trying to fill those holes as they come up, especially as we see more staff get infected, which, you know even with the best personal protective equipment and the best hygiene measures, it’s still out in the community and it’s still– you know, we’re still at quite a risk of exposure.
Marisa Wojcik:
So, as a health care professional, you are trained to manage a lot of different emergency situations. Do you feel prepared for this?
Kate Walton:
I mean it’s something that– maybe not specifics, but that we train for, right. So we always, especially in the emergency department, you never know what’s coming in the doors until it’s there. So, you know, we’re prepared for a surge or prepared for an incident with a lot of patients all at the same time. I think the different in this case from, you know, a normal snowy day with a lot of car accidents, for instance, is that this is looking to be a more sustained thing and the uncertainty really lies with how quickly this is going to spread and how much it’s going to amp up for us.
Marisa Wojcik:
What is, kind of, the mental health status of you and your coworkers? What’s the morale like and kind of where do you see that going if this is a persistent thing?
Kate Walton:
It’s interesting, I think we all sort of have our different ways of coping. We all have the things that that we already, you know, especially in emergency medicine, but I think throughout health care, we all have our ways that help us cope or de-stress. I have coworkers that have gotten really involved in just helping people outside of work so providing groceries for neighbors that can’t get out or who don’t want to, you know, like elderly neighbors who don’t want to be exposed. So I think that everyone’s sort of already have some coping measures and I think we’ve seen that sort of amping up a little bit, too, you know. And I’m kind of curious to see, like, the long-term community effects. So, as health care workers, you know, we expect to see fairly difficult things, but you know I’m concerned to see how this, especially if this social distancing and isolation goes on longer and the way people sort of cope with that.
Marisa Wojcik:
Yeah, I’m imagine for you to go from being in a very social situation at the hospital to self-quarantining at home. It’s kind of a drastic difference overall. Overall, not only are top officials trying to contain the virus, they’re trying to contain panic. How do you balance the line between conveying the seriousness of this, while also not instilling unnecessary panic with the public?
Kate Walton:
I think the thing for me, at least, the most helpful part of this is that there are things that we can do as a society to mitigate this to make it not a disaster. It will still be a challenge no matter what, but, you know, with social distancing and paid sick leave would be great. You know, that’s one of the things that I think is going to be the most challenging, is we’ve got, especially the larger corporations that aren’t giving paid sick leave to their employees or furloughing people and not paying them. But you know companies that if you’re sick, you can’t go to work. Especially in this case, it’s imperative that people don’t go to work sick. You know, and I see people all the time, that for them, that’s a decision between going to work sick or not being able to pay the bills because they don’t get paid if they don’t go, they don’t work. So, paid sick leave would be a great thing to help mitigate this and to help really with the community to make folks able to stay home and able to help practice for the good of public health, to not spread this virus.
Marisa Wojcik:
Kate, when is your next shift?
Kate Walton:
I work Friday.
Marisa Wojcik:
Alright. Well, good luck to you. Thank you very much for joining us.
Kate Walton:
Thank you so much for having me. I appreciate it.
Marisa Wojcik:
So, we’ll be keeping a close eye on this story and as it develops. This Friday’s “Here & Now” program, we’re going to be speaking with top health officials for the latest information statewide. For daily updates, visit PBSWisconsin.org and click on the ‘News’ tab. We’re updating all information there on a regular basis, including daily briefings, everything that you need to know, including election information, all sorts of good information there. So, visit that website and we will see you back here in a week. Thank you so much for joining us on “Noon Wednesday.”
Search Episodes

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport












Follow Us