Marisa Wojcik:
Welcome to “Noon Wednesday.” I’m Marisa Wojcik, multimedia journalist with “Here & Now” on PBS Wisconsin. We are back in the larger studio practicing good social distancing again this week. Lots of news for you. Really quick, as of 8 am this morning, the state of Wisconsin is under a shelter in place order, which Governor Evers is calling “Safer at Home,” and it’s meant to reduce the increasing spread of COVID-19 in the state. So what does that mean? Non-essential businesses are closed. People are allowed to leave their homes for things like going to get groceries, receiving health care. You can go outside, and you don’t need special permission, as long as you are following the exemptions under this order like groceries, going outside for a walk, whatever. So, in a press conference yesterday, Evers asked people to take this seriously, saying “No dinner parties, no sleepovers, no kids at the playground, no gatherings. We need you to be in physical contact with as few people as possible.” So, if you want more details on that order and general information about what is going on with Coronavirus in the state, visit PBSWisconsin.org/news. Lots of more information for you there. So why did the governor decide to do the shelter in place order now? As of last Friday, he told “Here & Now” that he would have great problems issuing a shelter in place order. So, this question leads us into our talk today. We’re talking about the urgent battle to flatten Wisconsin’s COVID-19 curve, which is the title of the newest piece by Will Cushman from WisContext and he joins us remotely now from his home. Will, thanks so much for being here. .. kind of.
[Will laughs]
Will Cushman:
Well, thank you for having me, Marisa. Happy to join you from my living room.
[Marisa laughs]
Marisa Wojcik:
So, as of right now, the Department of Health Services is reporting 457 confirmed cases of COVID-19, but their numbers generally update for the day around 2 pm so we expect more a little bit later. Five deaths. Last week at this time, the number was 72. So, how is this creating a curve? How do these numbers create what is being called “the curve”?
Will Cushman:
Yeah, that’s a really good question. So that, when we’re talking about flattening the curve or this, this curve, it is kind of like if you, if you if you don’t have a kind of basic understanding of what this is it might be kind of confusing. So, the curve is all about kind of plotting new infections over time. So, in this case, we’re thinking about new infections of COVID-19 in Wisconsin since the outbreak began in Wisconsin. So, we know that there is one confirmed case in Dane County all the way back to the beginning of February, and then, there’s about a month where there weren’t any new cases confirmed in Wisconsin. So, over that period, there were there wasn’t really a curve to speak of, but then it kind of in the first week of March– so not that long ago– we started to see more cases crop up in multiple counties across the state. And then, those new infections really started to rise pretty rapidly so that the curve in the growth of new infections in Wisconsin really became quite steep, quite quickly, and that is what is very concerning to public health officials and is precisely what is behind this “Safer at Home” order. The purpose of the order is to try to flatten the curve as we’ve been talking about. And flattening the curve means slowing down the rate of new infections over time.
Marisa Wojcik:
And so, literally, if you are looking at the data of infections over time, you are visualizing a curve going upwards and there’s some great visualizations from Will’s reporting on WisContext.org so check that out. But as officials are looking at this curve, what is their top priority?
Will Cushman:
Their main priority? So, that’s a really good question, as well, like what– why does it matter if suddenly, there are a whole bunch of people getting sick with COVID-19 at the same time? I think a lot of people might especially be wondering that since we keep hearing that the majority– upwards of 80% of people only get mild or moderate symptoms. What the real big problem is with COVID-19, is that about one in five, one in six, so around 20% of patients require hospitalization. They’re so sick that they require hospitalization and then about a quarter of those patients require ICU care, maybe a ventilator. And these are very limited resources, not only in Wisconsin, but pretty much everywhere. So, the whole effort to flatten the curve to slow down the rate of new infections is to protect our health care system and to make sure that there are never so many people sick with COVID-19 at the same time that all those sick patients overwhelm our hospitals.
Marisa Wojcik:
And yesterday, DHS Secretary-designee Andrea Palm said that they are looking at all of this data in Wisconsin and comparing it to experiences in Wuhan and Italy. So, what are they looking to compare? What kind of information are they– are they trying to garner to make these decisions?
Will Cushman:
Yeah, they are looking at kind of how COVID-19 has played out in places where outbreaks are at this point fairly mature. So, they’ve been going on for a while. So what they saw in Wuhan was a pretty rapid– that that’s where the COVID-19 originated and in Central China, what they saw there way back in January when it started, it was a pretty rapid rise in new infections so a pretty steep curve but then also a whole number of social control measures, including like a whole lockdown of the whole region around Wuhan and that really and a whole bunch of other mandates related to social distancing that are a lot more stringent than they are here and what they saw there was a decline in the rate of new infections over time, so to speak flattening of that curve. In Italy, the– we’ve also seen in Northern Italy in particular, when that outbreak really got going it also– the curve associated with it, so the curve of new infections over time, it’s really quite steep and it took a while for that to flatten because as we saw in Italy, it took a little bit longer for some of those orders, those social distancing orders, the lockdowns to take effect and for people to take them really actually quite seriously. And so, our public health officials are– they’re looking at those cases and seeing that really the only way to protect our hospital system’s capacity to deal with patients is to reduce the number of or the rate of new infections over time. We see in Northern Italy that their hospitals around Milan are quite overwhelmed at this point and they’re having to prioritize who to treat and who to put on ventilators. That is obviously a wrenching decision for doctors to make and something that officials want to avoid here in Wisconsin.
Marisa Wojcik:
And as you mentioned, State Epidemiologist Ryan Westergaard said that with mild and moderate symptoms for the majority of people that does still translate into concern for everyone else. That can be a little bit difficult to understand because if the majority of people are experiencing mild or moderate symptoms, then why are we concerned at all about the general population?
Will Cushman:
Yeah, that’s a good question too, and I think the flip side here is because so many people experience such mild symptoms, symptoms that might be akin to a mild flu or even a mild cold, the concern is that they, without a safer at home order or a social distancing mandates, so to speak, may just go about their lives kind of as they otherwise would with a common cold, which we know a lot of people are quite used to going shopping, going to work, picking up their kids from school, all of that while having a minor illness. It’s maybe not the best thing to do, but I think most of us have done that before and so the concern is that those people with mild or moderate symptoms can very easily be spreading the disease quite widely. We know that the contagion is very rapid. It’s more rapid than influenza and so the concern is that really an outbreak could become out of control quite quickly basically, because it’s being spread by people with mild symptoms and then if enough people catch it, there is going to be a fair number of people who do require hospitalization and the fear is that that number could be so high that it would overwhelm our hospitals.
Marisa Wojcik:
In a media briefing yesterday, State DHS Secretary-designee Andrea Palm also said that if we continue on our current path without implementing Safer at Home to flatten the curve, the models show us we would have 22,000 Wisconsinites positive for COVID-19 by April 8 and anywhere between 440 and 1,500 deaths. What is the capacity of our hospitals to manage patients whether or not we are implementing Safer at Home? Do we understand where those numbers are at right now?
Will Cushman:
It’s– that’s a really good question and one to which the answer is kind of constantly changing right now. We know that hospitals are doing everything they can to free up capacity so they’re canceling elective procedures, trying to keep people who might otherwise come to the ER or go to the doctor for reasons that could be taken care of via telemedicine, they’re trying to keep them at home, basically doing everything they can to keep as many beds free for COVID-19 patients. We know that those resources are limited. There are about 2,500 ICU beds in the state. There are only a little bit over 600-some ventilators in the state and with the state of a population of nearly six million, if a good portion of that population gets sick quite rapidly, there are going to be more people requiring ICU beds and ventilators than they’re simply is capacity and just even looking at basic numbers of all hospital beds. So, not even considering ICU beds, Wisconsin is kind of doing a little bit better than the national average, where there’s 2.8 hospital beds per thousand people in the US. In Wisconsin, it’s 3.1 hospital beds per thousand people roughly. And that number may be a little bit changed, or changing now as hospitals beef up capacity but I think there are a whole lot of things that complicate comparisons between Wisconsin and Italy. Our populations are different. Our health systems work differently, but at a very basic level, so we have 3.1 hospital beds per thousand people in Wisconsin. Italy has 3.2 hospital beds per thousand people. So, in terms of just kind of like fundamental capacity to deal with a huge spike in serious illness, I think Wisconsin is in a kind of precarious position.
Marisa Wojcik:
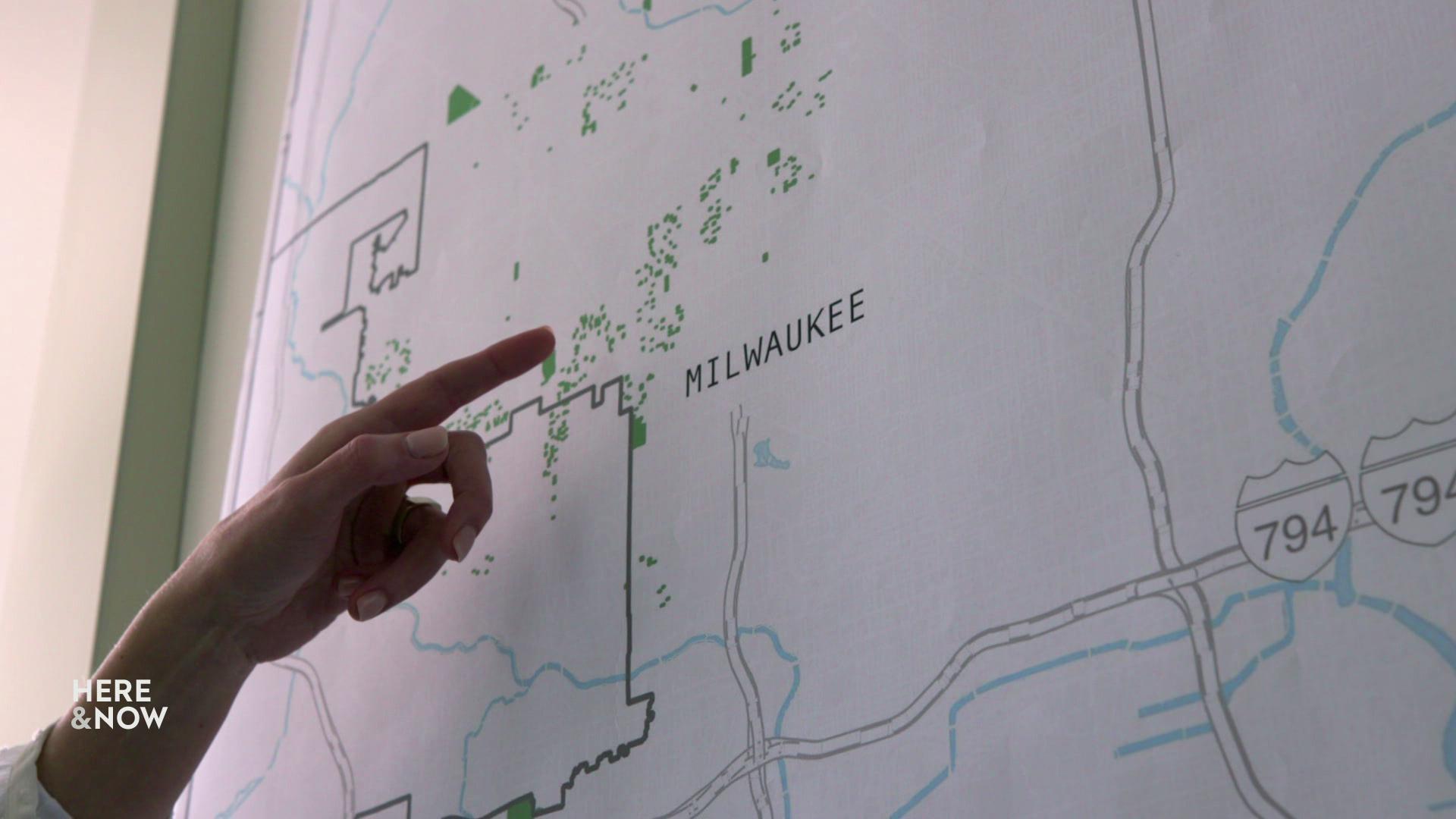
And your story has projections of hospital beds that are available versus what the actual need will be based on percentages of the population contracting the virus. So, generally what did those projections show?
Will Cushman:
Yeah, so we were looking at data from Harvard, actually, a group of researchers at Harvard, who worked with “ProPublica” and “The New York Times” to kind of disseminate this study. But then they made all of their data publicly available to anyone so that was that was great for us. They looked at kind of the capacities of what are called the hospital referral regions. These are large regions that are– mostly health care researchers care about what a hospital referral region is. Like, you or me or anyone in Wisconsin who’s a patient doesn’t really necessarily care about this, but the regions themselves are kind of large geographical areas that are anchored by at least one hospital that has kind of major health care capabilities, so cardiovascular and neurosurgery capabilities. In Wisconsin, they’re associated with the larger cities so Milwaukee, Madison, Green Bay, Appleton, Wausau, and then a whole bunch that are there–there’s a whole bunch of others and then several that are associated with cities in neighboring states, as well. And so what these researchers did was look at the number of hospital beds that are in those referral regions and then also looked at data about the average number of hospital beds that are occupied at any given time and for most of those referral regions, the average occupancy at any random point in time is somewhere around 50% and then they wanted to– these researchers wanted to model the effects of a COVID-19 outbreak that infects 20% of the adult population, 40% of the adult population, and 60% of the adult population, and they also wanted to model the effects of social distancing mandates or if we just went about our daily business as if nothing is happening. And what they found is that if we were to go about daily life pretty much normally and about 60% of the adult population were to contract COVID-19, which is a very real possibility, that many of our regions would be woefully overwhelmed. So, the region around Appleton, for instance, like the Appleton region’s hospitals would be the– their capacity would be exceeded by 500% with COVID-19 patients and the similar numbers are kind of like throughout the state and all these regions would experience similar capacity issues. Even with major social distancing and a smaller percentage of people contracting COVID-19, these models predict that our– many of our hospital systems will be quite strained, but they would be able to handle the influx of COVID-19 patients better, but it would still be a struggle pretty much no matter what, even in a best-case scenario.
Marisa Wojick:
And Dr. Westergaard predicted yesterday that of the 457 cases that are positive in Wisconsin, about 20% of those 457 are hospitalized right now. Just to give a little bit of a lay of the land of what they’re predicting for the state of things at the moment. What about the hospital staff and health care workers? Is that part of the modeling projection to make sure that we can handle what’s coming?
Will Cushman:
That’s a really good question. That wasn’t a piece of the modeling that the Harvard researchers published and that I looked at. I do know that other studies that have come out have pointed to maybe the most critical resource that could be lacking in some places is the number of health care workers that are available to give care. Particularly, respiratory therapists are in quite short supply. Pretty much everywhere, there aren’t a ton of respiratory therapists and we know that they’re extremely important in responding to critical respiratory illness, such as critical COVID-19 cases so that is a worry. And I do know that the state is working on ways to try to not only expand capacity in terms of hospital beds and ventilators and medications and all that, but also trying to get people who have come– who have retired– trying to get them to come out of retirement temporarily to assist– so that would be retired health care workers– and trying to figure out other ways that we can get as many health care workers in our hospitals helping patients as possible.
Marisa Wojcik:
So, the broad decision to order people to stay home, all has to do with flattening the curve and that means slowing down the rate at which the virus is spreading, but does that mean if we extend the timeline eventually, we’ll still see the same number of cases just over a longer period of time?
Will Cushman:
Yeah, that’s another really good question, and I think something that a lot of people might be curious about. Like it does seem like, “Okay an order like this, a safer at home order or shelter in place order, you might think it’s all about keeping people from getting sick ever and that’s not necessarily what it’s all about. I– obviously, doctors and public health officials would like to reduce the burden of illness on the population as much as possible. So we want to reduce the number of people who get sick ultimately from COVID-19, but the real goal of a shelter in place or a safer at home order is to not necessarily reduce the total number of people who get sick from COVID-19 ever, but to spread out that illness over a longer period of time. That might also sound kind of counterintuitive. Like, why would you want the outbreak to last longer? I think a lot of people like myself who are kind of cooped up in our homes are thinking about that, and they’re like, “Oh, gosh. I don’t want this to last longer.” But the real issue is that if it if it doesn’t last longer, than there will be a lot more people sick all at once, and that is–the real fear is that can overwhelm our capacity and therefore more people would die.
Marisa Wojcik:
Alright well, thanks very much for joining us.
Will Cushman:
Thank you, Marisa.
Marisa Wojcik:
For more from with WisContext and Will’s story about flattening the curve, there’s lots of really detailed information in there so you can comb through it. Will do a lot of research. You can visit WisContext.org. That’s WisContext.org. This Friday on PBS Wisconsin at 7 pm, we are going to bring you interviews with two candidates from the state Supreme Court, and speaking of which, right now, Wisconsin is still planning on having an election on April 7th. The presidential preference primary, State Supreme Court, and local offices will all be during the April 7 Election. You can still request an absentee ballot if you don’t want to vote in person. And on this Friday’s “Here & Now” at 7:30, we’re going to be bringing you more information about COVID-19 in Wisconsin. And, as always, you can find more at PBSWisconsin.org/news. That’s PBSWisconsin.org/news. We have tons of articles and more information for you, rich with a lot of stuff that you can find there. And we’ll see you back here in a week. Thank you so much for joining us on “Noon Wednesday.”
Search Episodes

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport












Follow Us