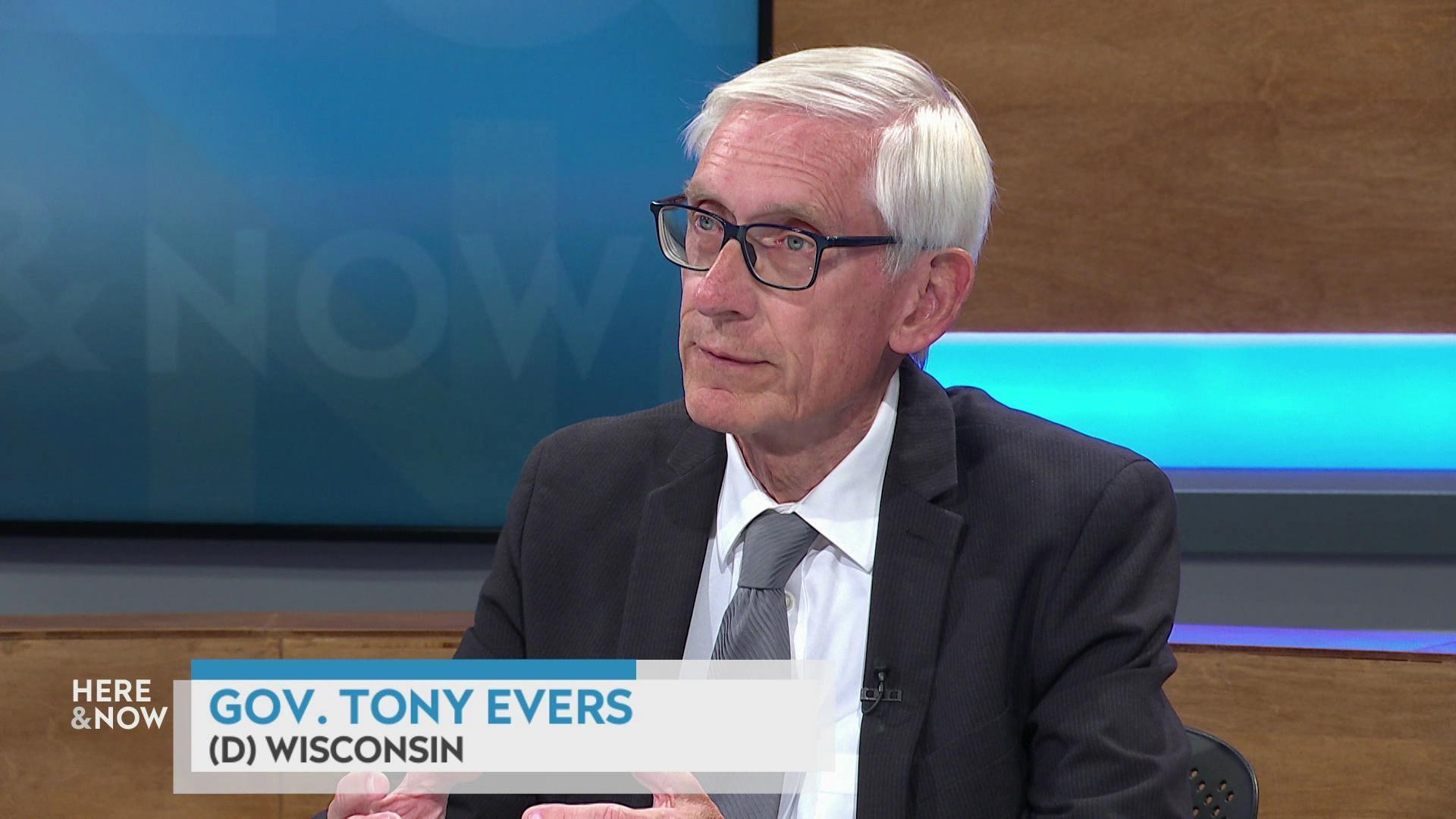
Frederica Freyberg:
The COVID pandemic is in the rear view for most of us, but is it? There’s a new variant circulating and several counties in Wisconsin report high concentrations of the virus in wastewater right now. Still, it’s nothing compared to the worst days over the last three years. Are we as a nation and a state prepared for the next pandemic? We turn to Dr. Michael Osterholm, formerly a Biden White House adviser on COVID, for his take. Thanks for being here.
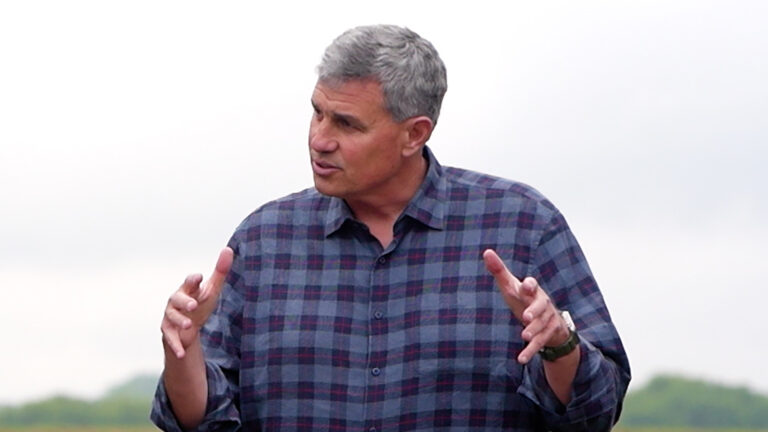
Michael Osterholm:
Thanks. Good to be back with you again.
Frederica Freyberg:
So you say it’s not done with us yet. Why do you say that?
Michael Osterholm:
Well, first of all, I’m quite convinced that the big pandemic thrust that we saw from 2020 to 2023 is, in fact the pandemic behind us. What we’re really dealing with now is what will it look like going forward? Just like if you have an influenza pandemic. It’s a new virus. It causes real challenges for several years and then it basically adapts into the seasonal flu pattern. What we don’t know with COVID yet is what it will look like? Is it a seasonal virus? Well, right now it’s occurring in all four seasons. So I guess you can say in that regard it’s seasonal, but does it look like anything like the respiratory viruses like influenza or RSV we see? No. Do we see cases increase in the summer? We have. We’ve seen them increase in the fall. So we’re really unclear yet what this pattern is going to look like, but it’s very, very clear that the virus is still here with us.
Frederica Freyberg:
So you and fellow White House advisors wrote about your take-aways from the pandemic, including that as a nation, we should prepare now for whatever might come next, but didn’t our experience of COVID result in stockpiles of scientific knowledge, infrastructure, personal protective gear and all of that?
Michael Osterholm:
Well, you know, this is at best a very complicated topic. For example, you mentioned respiratory gear. One of the challenges that we had is early on a number of us recognized that this virus was being spread by what we call the airborne route, just breathing air that would move through a large room. And yet we had many who continued to use surgical masks, the kind of masks that are not tight fitting around the face, and while they may have thought they were protected or they were protecting others, they really weren’t. And so we still have many hospitals that are using outdated respiratory protection gear some three years after they should have switched to N95 respirators. So there we’re not really prepared. We still have a lot of work to do. I think the other thing that really is challenging is that public health has, as a discipline, always relied on basically the trust of the people. The belief that, in fact, you know, we were doing what was right for the population to protect them against, in this case, a virus. We’ve lost a lot of the trust and the support of the public over the last several years because they felt like we were not being truthful when we should have said we don’t know. We made statements that suggested we knew more than we did and then it turned out to be wrong, and so I think we have a lot of work yet to do for the next pandemic. And if I had to give you my best professional judgment, I would say we’re less prepared for a pandemic today than we were in 2019.
Frederica Freyberg:
It just doesn’t seem possible that that’s true with all of the efforts, including your own, that went into this during the worst days of the pandemic. But as to the public trust in public health, can that be regained?
Michael Osterholm:
Well, I think it can be regained, but we have lessons to learn and we have to realize we’re in a very different world today than we have been for the last hundred years with regard to how public health is viewed. I mean, we need to look no further than our political climate today in this country to understand the distrust, the mistrust in so many establishments or institutions of our society, and that is really a crisis. When somebody says you must evacuate now. You must get out now. That is not up for discussion or debate, but people will only do that if they trust that what you’re telling them is true. Now, we don’t have to evacuate for a pandemic, but we want, for example, people to get vaccinated. In this country, only 42% of the people who are at high risk for serious illness, hospitalizations or deaths, got the booster dose over the last year, and I think with the new booster dose that’s coming out in the next few weeks, an even smaller percentage of those who are at risk for serious illness are going to get evacuated. Why is that? Why would someone not take a lifesaving, and if nothing else, at least reducing your risk of serious illness vaccine? What have we done that has led people to not want to get those? So I think we still have a lot of work to do to understand that, and I keep saying time and time again, the first and most important lesson we should have learned is the critical, critical nature of humility. What do we know? What do we don’t know. What we know, how do we know it? And what we don’t know, what are we going to do to find out? And so I think that that’s still is a major lesson that we should all take home from this pandemic.
Frederica Freyberg:
I don’t have much time left, but I do want to ask you about another one of your important takeaways, and that is that schools should not be shut down except in rare cases, but I ask was not the COVID pandemic a rare case?
Michael Osterholm:
My message has always been is we should be basing what we do on data. Are we seeing infections in schools? If so, we may need snow days. We may need to take some time off to let the virus in a community basically come down some, but where we don’t see evidence of ongoing widespread infection, then we shouldn’t be closed down. And what we did was just put in blanket “do this or do that” without really understanding how we had to react to what was happening in the community. What are the data supports? In the period of 2022, early 2023, I thoroughly supported closing schools with omicron. We had up to half the teachers out sick. How do you provide education, and, of course, we worry about the kids, but in that first year of the pandemic, frankly, having closed schools was not likely anything that provided additional protection for the community. So this is, again, another very complicated message that public health has to get better at sharing why do we do what we do and why don’t we do what we don’t do.
Frederica Freyberg:
Dr. Michael Osterholm, thanks very much.
Michael Osterholm:
Thank you.
Search Episodes

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?
Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?
Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport














Follow Us