Frederica Freyberg:
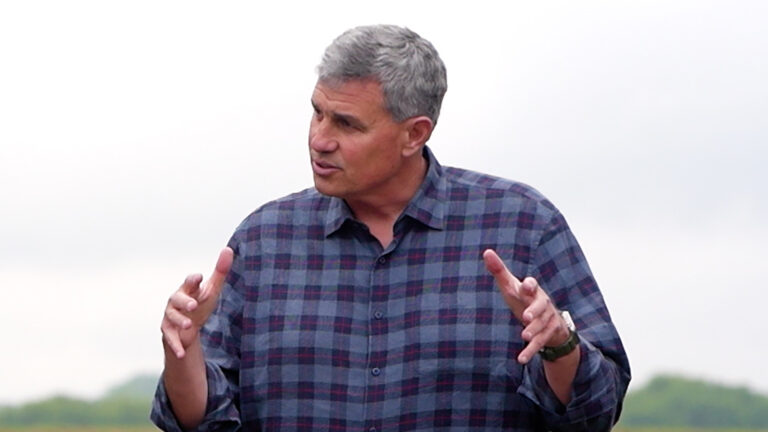
But first this week, the state Department of Health Services announced that more than 80,000 childless adults gained Medicaid coverage this year. Of those there were about 19,000 new people insured under the state’s program known as BadgerCare. What’s not known yet is what becomes of the more than 62,000 adults who lost Medicaid coverage. Those would be adults whose annual income is just above the poverty line. We go over the numbers now with the deputy secretary of Health Services, Kevin Moore. Thanks very much for being here.
Kevin Moore:
Thanks for having me.
Frederica Freyberg:
So was your agency surprised by the larger than expected number of people who were eligible and signed on to BadgerCare?
Kevin Moore:
The response from the department was that we had expected to have about this number of people enrolled. Some of the enrollment took a little bit faster than what we had initially projected. But overall we’re pretty close to where we expected to be for overall enrollment numbers, with almost 100,000 people total coverage and then as we announced today, 81,000 new childless adults that didn’t have access to coverage before because they were living in poverty now have access to BadgerCare. So we think that we’re on track. We’re based on where we think our final numbers are. And we’ll continue to monitor it in the weeks and months ahead.
Frederica Freyberg:
Now I know that the administration and your agency, you continually say that Wisconsin is the only state to not take the expansion of Medicaid, with no health coverage gap. But how do you know whether or not you will have a health coverage gap until you find out how many who lost Medicaid have actually signed on to the Affordable Care Act marketplace?
Kevin Moore:
Yeah. I think it really comes down to looking at the federal law and the federal Affordable Care Act and then the Wisconsin policies, and looking at how those two intertwine. If you look at the federal Affordable Care Act, they provide subsidies in the health insurance exchanges to people 100% of federal poverty and above. In Wisconsin, Medicaid then would pick up from 100% and below. What's also interesting is that he Affordable Care Act doesn’t provide subsidies for people below 100% of federal poverty. So for those people in Wisconsin, we truly– We plug that hole. And then for those people above 100% then the exchanges are optional. And again, through the Affordable Care Act they get the subsidies and the cost-sharing that can help it make more affordable for their families.
Frederica Freyberg:
So the state arranged it so there would be no gap if these people who were transitioning off BadgerCare did in fact avail themselves, and didn’t somehow give up or something when the website was bad.
Kevin Moore:
And that’s part of the reason why when the state decided to postpone a lot of these changes from the beginning of the year for three months and, again, that was because of the challenges with healthcare.gov. The reason why the policy was designed was the affordability determination was part of the federal law. It was said that for folks above 100% of federal poverty, they could purchase health insurance through the exchanges. So it was– The plan was to make sure that there was no gap, to take care of those in poverty, which through Governor Walker’s reforms we were able to do so. But then for those above and beyond it really becomes, both the federal law and state law basically said– We can’t force people and force families to make those decisions. They have to determine whether or not it is truly affordable for them and their family. And again, it’s based off the federal determination of affordability by the law. So I think for us we wanted to set the stage. Our outreach efforts were robust to make sure people transitioning, but also people who weren’t in Medicaid. Again, it's important to note that subsidies went to people all the way up to 400% of the federal poverty level.
Frederica Freyberg:
What is the status today on delivering the number of people who lost BadgerCare and signed on to marketplace coverage?
Kevin Moore:
We just recently got the data from CMS, the Centers for Medicare and Medicaid Services, and we are continually looking through that data to determine exactly what that number is. We don't have that number exactly. We’re also identifying, as we look at that data though, there are other issues about perhaps people that may have been in the transition population, they may have moved back into Medicaid. Something may have changed in their eligibility and their income level. We want to double check that as well, to determine whether or not they are truly transitioned, or did they come back in. Another thing to keep in mind is that for many of these folks, they may have gone back on their employer-sponsored health insurance. Wisconsin had a very high eligibility level at the 200% of federal poverty for many of the people in the transition population. For those individuals, they may have looked at the exchanges and realized it was more cost effective to go back on a spouse’s plan or get insurance through their employer.
Frederica Freyberg:
You’re crunching these numbers, people over at Health Services. Can you give me any sense, preliminarily, of whether or not these numbers are going to reach that kind of 90% threshold which I think the governor has said he would think was successful?
Kevin Moore:
I think we are a little bit too early to be able to give you that type of indication, primarily because of a lot of these different things that we’re talking about. The ability to purchase health insurance through the marketplace or through the exchange was only one way that people could get coverage. And we want to make sure that we’re giving the most full answer to that, not giving a snapshot that could be taken out of context or actually not truly reflect whether or not people have coverage. I think it's just safer to say we want to continue to look at those numbers before we give out anything that might be half truth.
Frederica Freyberg:
People, as you know, however, are getting impatient for the delivery of these numbers. In fact, US Senator Tammy Baldwin continues to call for the quick release of them saying, Your decision to reject the federal investment in our BadgerCare program put health coverage for thousands of Wisconsinites at risk, and I continued to be concerned that your plan, which covers fewer people at a higher cost to taxpayers, will result in people becoming uninsured. To ensure that your plan will not create a gap in coverage for Wisconsin, it is critical, she says, that we know if the nearly 63,000 of our fellow citizens have seamlessly transitioned from BadgerCare to the marketplace before, she says, the end of the month. So what is your reaction to the senator’s comments?
Kevin Moore:
I think at the end of the day, and I'll just reiterate this, that the senator brings up some very important parts. It’s part of the reason why we greatly appreciated when she called for help with CMS to get the data, do the data match. We appreciated the fact that she stepped forward. But as I mentioned before, the ability for us to take a look at the data of the people that purchased in the exchange is just one option that families may have taken. Again, I go back to the fact that there are a lot of individuals who may have had access to employer-sponsored health insurance but chose BadgerCare instead. They’re going to go back to their employer or their employer-sponsored health insurance. And the reality is that’s not going to be reflected in the data because they’re not going to have purchased through the exchange. Or the other option is that people didn’t have to buy in the exchange. They could have purchased outside of the exchange as well. So again, that’s part of the reason why, with all due respect, we want to make sure that we provide the taxpayers and the residents of the state of Wisconsin with the full database, the full information. And also understand that that’s going to be incomplete because there are going to be instances where people may have made decisions that may have found that the exchange was not as affordable as it was deemed by those who are supporters of it and realize that perhaps another option either through a spouse or through an employer might have been a more affordable option to get coverage for their family. All of that is part of those numbers and part of the reason why we’re being very cautious and very respectful. Because we want to make sure the public gets the most accurate data.
Frederica Freyberg:
All right, and we expect to see those, when then?
Kevin Moore:
We’re hoping within the next couple weeks as we continue to crunch through. And barring any oddities in those numbers, like I said, sometimes we’ve actually seen that there are individuals because of the fact that their income may have changed, they may have actually become eligible for Medicaid again. So we want to make sure we have the best data available. So I'd say within the next few weeks.
Frederica Freyberg:
All right. Kevin Moore, thanks very much.
Kevin Moore:
Thank you for having me.
Search Episodes
News Stories from PBS Wisconsin

Donate to sign up. Activate and sign in to Passport. It's that easy to help PBS Wisconsin serve your community through media that educates, inspires, and entertains.
Make your membership gift today
Only for new users: Activate Passport using your code or email address
Already a member?
Look up my account
Need some help? Go to FAQ or visit PBS Passport Help
Need help accessing PBS Wisconsin anywhere?

Online Access | Platform & Device Access | Cable or Satellite Access | Over-The-Air Access
Visit Access Guide
Need help accessing PBS Wisconsin anywhere?

Visit Our
Live TV Access Guide
Online AccessPlatform & Device Access
Cable or Satellite Access
Over-The-Air Access
Visit Access Guide
 Passport
Passport















Follow Us