When COVID-19 is endemic, what's the role of testing?
As the pandemic has shifted to a prolonged phase, the role of tests to measure the presence and breadth of infection is changing as well to keep up with a more complex situation.
July 12, 2022

(Credit: Steven Potter/ PBS Wisconsin)
In the first few months of the pandemic, testing for infection was the holy grail of COVID-19 prevention and protection. In early 2020, tests were relied on to not only safeguard others but also to track how rapidly and where the SARS-CoV-2 virus was spreading.
But over the next couple of years, a lot would end up changing.
Halfway through 2022, there are multiple covid vaccines, widely available and effective in reducing the risk of serious disease, and more options are in development. Directives on when and how long to isolate after contracting the virus have lessened. Masking has gone from largely mandatory to largely discretionary and restrictions on public gatherings have been eliminated. For those who do get sick, there are antiviral treatments to help people recover.
As for testing, a variety of at-home rapid antigen test kits – the less-accurate-but-faster-results counterpart of professionally-administered molecular-level PCR tests – have become widely available. So available, in fact, the federal government will even mail antigen tests to homes for free.
Given all of these gains, there are extensive discussions in medical communities about the public health transition from a pandemic stance to a less-severe and less-disruptive endemic status. And that shift means COVID-19 testing – frequency, importance, reliance and public perception – is likewise changing.
Understanding the path forward on testing is immediately pertinent as the United States is in the midst of yet another coronavirus wave from yet another subvariant – omicron BA.5 – which has been found to be even more elusive to the immune system than previous mutations.
As of mid-July 2022, the Centers for Disease Control and Prevention is reporting just over 100,000 new COVID-19 cases a day across the nation, but public health authorities warn that that number is likely to be seriously underestimated given many people are testing at home or not testing at all.
Three reasons to test
Ryan Westergaard, state epidemiologist for communicable diseases with the Wisconsin Department of Health Services, said COVID-19 testing is “still very important” but added that “it’s important in different ways than it was two years ago.”
There are three reasons why testing is still needed, he said. First, in order to receive antiviral medications – such as Plaxlovid – to treat COVID-19, infection by the virus has to be proven in a patient.
Testing is also important for higher-risk patients. “If someone is at risk for severe COVID-19 pneumonia or the kind of illness that requires hospital care or ICU care, getting a positive test is the first step in the process of getting the care that they need,” explained Westergaard. “We need to test people, so we can treat people.”
Westergaard said a second reason to maintain testing is “to support our awareness of what the epidemic is doing and the general epidemiology,” meaning the locations and rate that the virus is spreading.
“It’s no longer as important to know the precise number of people with infections. But we do need to know where the virus is to protect those who are at high risk and to be able to give public health recommendations,” he said. “We don’t need to test 100% of cases to have that information. We need to do enough sampling to have a meaningful estimate of what it is and be able to track trends over time.”
Westergaard likened this change in the need for testing to estimates used in weather forecasting.
“We have weather stations and sensors in a lot of different places, but not in every single person’s backyard,” he continued. “But we can predict what’s happening with the weather in good detail by sampling in just the right amount.”
Lastly, Westergaard said testing is needed to keep track of how the virus is mutating and changing.
“The virus is continuing to evolve, and we need to monitor what variants are circulating and be able to detect new variants,” he said, adding that this kind of “genomic surveillance will be going on with this virus forever and the way that we get information about that is to test people.”
Testing frustrations
When it comes to variants, such as delta or omicron, and subvariants such as the latter’s BA.4 or BA.5, Westergaard noted that viral mutation may make existing tests obsolete or, at the least, increasingly less accurate.
“At-home tests and antigen tests have never been perfect and they may be getting less perfect over time as the virus evolves,” he said, adding that inaccuracy caused by mutations only add to the problem many have encountered with testing negative when they actually do have COVID-19. “We don’t have complete data to see how much the accuracy of tests has gone down over time as the virus has evolved, but it remains true that even if someone is truly infected, an antigen test can be negative.”
The problem of false-negative test results – caused either by a too-low viral load or a test user error – with at-home tests has caused a lot of frustration by test takers, which, in turn, has led to numerous social media complaints and discussions questioning testing efficacy. These circumstances mirror, in many ways, a similarly shifting situation with vaccines.
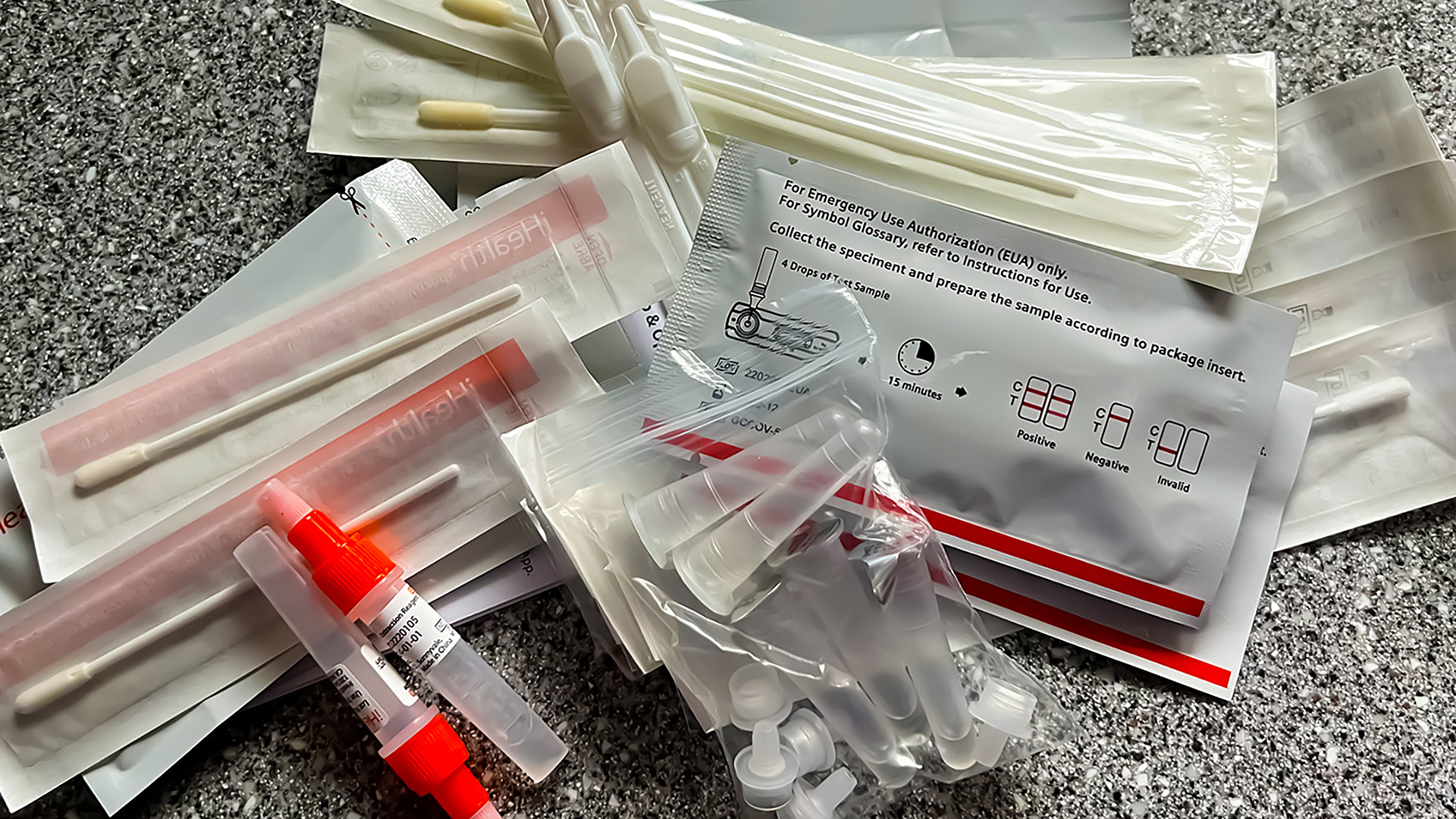
At-home antigen test kits have become increasingly relied upon by people trying to learn if they have become infected with COVID-19. (Credit: Steven Potter / PBS Wisconsin)
Westergaard wouldn’t speculate about any possible decline in public confidence in testing due to these inaccuracies. Instead of discounting the need for testing, he said, it’s necessary to adjust the value placed in testing.
“I think people should think about COVID testing as less unique or exceptional than it was before and think about it as an important part of health care that everyone should have access to,” he explained.
That said, as the endemic phase of living with COVID-19 continues, testing will increasingly become most important for those who have the greatest risk of developing serious or deadly complications from infection.
“The symptoms of a COVID-19 infection are very similar to influenza and other respiratory viruses. If someone develops that kind of illness, it’s not wrong to get a test because if you’re positive, [it] can help keep you and others safe,” Westergaard said. “It’s probably not essential that every person, every time get tested, but there are some people that really should get tested if they develop symptoms and that’s people who are at high risk of getting very sick and could benefit from treatment.”
So, what circumstances warrant more attention to testing?
“People who are unvaccinated or who have chronic health conditions that would put them in that category of being a higher likelihood of needing to be hospitalized – they should get tested any time they have a covid-like illness,” Westergaard said.
Future testing
Looking forward, Westergaard sees endemic COVID-19 as a chance to improve the technology and reach of testing.
“What I hope happens is for us to move toward what some people call multiplex testing. We have tests that can detect influenza and tests that can detect SARS-CoV-2 and we have tests that can detect a panel of 11 different viruses. But they’re not used very much because they’re expensive and they require specialized equipment,” he explained. A catch-all multiplex test, though, could detect which virus a patient has from among many that have similar symptoms.
“It would be nice to be able to name what’s making us sick with more regularity and more reliability than we have now. We’ve taken a good step in that direction by having a lot of covid tests out there. And the technology exists where we could diagnose any number of viruses,” said Westergaard. “Given that we’ve had to live through the pandemic and are more accustomed to getting a test when we get symptoms that could be covid, there are benefits for where we could get tested for all kinds of diseases.”
 Passport
Passport









Follow Us